Is It Time for a Telehealth Strategy?
Survey finds telehealth will grow 37% from pre-COVID levels when PHE ends, indicating a pressing need for telehealth strategy.
Healthcare had two big surprises in 2020: the rise of COVID-19 and the quick adoption of telehealth. Telehealth became a critical tool for patient access to care during the public health emergency (PHE) and a financial lifeline for providers struggling to remain open during lockdowns.
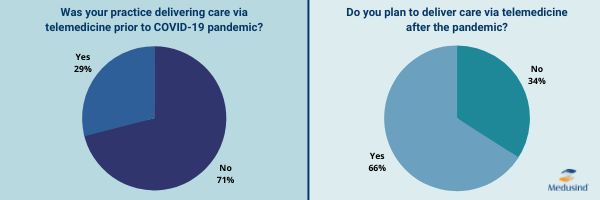
There is no doubt that the pandemic accelerated the growth of telehealth, and now it is clear the surge in telehealth will last. According to a recent survey by Medusind of its healthcare practices using telehealth during the PHE, 66 percent plan to continue delivery of telehealth services after the pandemic, a growth of 37 percent from pre-pandemic levels.
Perhaps one reason for the quick uptake of telehealth was that almost 60 percent of those surveyed had access to a telehealth platform either through a dedicated vendor or through their EHR system. Another reason may be the support practices had from partners that were invested in their performance.
“When you look at the user story for telehealth, both from a provider’s perspective and the patient’s perspective, it’s all about access to care,” shared Medusind CEO and Group President Vipul Bansal. He continued, “Prior to the PHE rules for telehealth reimbursement, though, most providers did not have access to this revenue stream except under specific conditions. With the preponderance of telehealth technology and strong patient demand for remote care, I am hopeful that it will remain a viable mechanism to deliver outcomes for our clients.”
Almost 24% of respondents had no major challenges with telehealth
Providers’ comfort level with using telehealth services has grown as well. Before the pandemic, approximately one-third of providers classified telemedicine as easy or very easy to use. Now, the majority (69 percent) find it easy or very easy.
In addition to building competence, many providers reported the integration of telehealth into their practices went smoothly. When asked about specific challenges of telemedicine, less than 10 percent found telemedicine workflows or technology challenging. Almost 24 percent reported they had no major challenges.
“My organization ‘turned on’ telehealth for our patients at the outset of the PHE and we were surprised at how quickly providers and patients adapted to the new normal,” shared Justin Gularek, COO/Executive Director of South Florida Surgical Specialists, LLC. Justin continued “We prepared for challenges on both ends of the screen but there were no notable setbacks. A lot of this, I think, is that we’re living in a world where so much technology is embedded into our daily lives that nearly everyone intuitively understands the experience.”
Building telehealth into strategic planning
Since telehealth is here to stay, some healthcare leadership is beginning to incorporate telehealth into their strategic planning, rather than considering it as something ‘on the side.’
There are several questions to consider when creating a strategic plan that includes telehealth:
- Where does telehealth work best for your practice?
- What are the organization’s goals, and what role can telehealth play?
- Should the organization consider setting specific telehealth goals, or should planned goals be re-prioritized?
- What is the definition of a successful telehealth program?
- Should there be staffing or schedule accommodations for telehealth?
- How can telehealth policies, regulations, and coding be kept up to date?
Not to be overlooked in planning is the role telehealth can play in keeping costs down while making healthcare more accessible and efficient. Some practices may want to consider marketing their telehealth services to increase market share and cultivate another revenue stream for their organization.
Like any new endeavor, telehealth growth will bring risks and challenges. However, many patients and providers would agree that an optimized telehealth program not only has the potential to improve patient outcomes but can also improve physician efficiency, time management, and ultimately the bottom line.
The best path forward will involve a collaborative approach between patients, providers, and provider support organizations.
___________________
About Medusind:
Since 2002, organizations across the entire healthcare spectrum have leveraged Medusind’s deep expertise and high-quality RCM solutions to maximize revenue, reduce operating costs, and navigate the changing healthcare landscape.
Click to learn how Medusind’s powerful technology and tailored Revenue Cycle Management services deliver outstanding financial results for healthcare organizations nationwide.




