revenue cycle management (RCM)
What is revenue cycle management (RCM)?
Revenue cycle management (RCM) is the financial process, utilizing medical billing software, that healthcare facilities use to track patient care episodes from registration and appointment scheduling to the final payment of a balance to ensure proper identification, collection and management of revenues from patient services.
What is healthcare revenue cycle management?
Financial stability is critical for healthcare organizations to stay in the business of helping patients. To ensure profitability and financial viability, they must properly collect and manage revenue. Equally important is having full visibility of their revenue cycle and revenue generation practices and processes, including billing, payment and claims processing. That's where revenue cycle management comes in.
RCM is the process of managing all revenue-generation functions in a healthcare organization. It requires an understanding of the revenue cycle and begins when a patient seeks the organization's medical services and ends when the organization has collected all payments from the patient and/or their insurer.
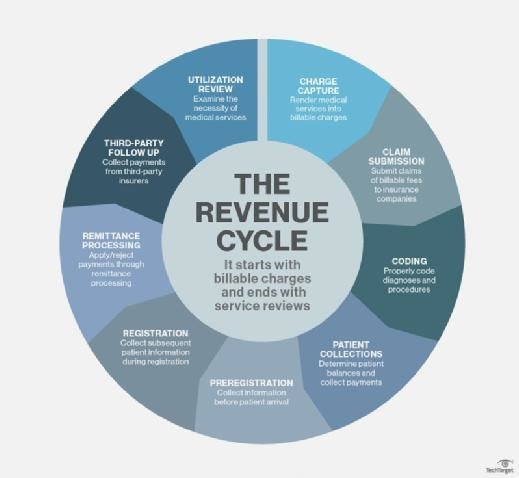
The revenue cycle in healthcare
In healthcare, the revenue cycle includes all the administrative and clinical functions that contribute to the capture, management and collection of patient service revenue. The following activities are involved in the revenue cycle: charge capture, claim submission, coding, patient collections, preregistration, registration, remittance processing, third-party follow-up and utilization review.
This article is part of
AI in healthcare: A guide to improving patient care with AI
The importance of data in revenue cycle management
RCM unifies the business and clinical sides of healthcare by coupling administrative data, such as a patient's name, insurance provider, insurance coverage and other personal information, with the treatment a patient receives, their medical history, and any available healthcare data (preexisting health conditions, allergies, lab test results, etc.).
Creating a patient account that includes data from the initial appointment setting can help simplify the organization's revenue cycle. Preregistration -- the collection of information before patient arrival -- brings clarity into the cycle, reduces the probability of time-wasting rework and helps optimize RCM.
Revenue cycle management and insurer communications
Communicating with health insurance companies is a key component of RCM. When a patient schedules an appointment, the physician's office or the hospital staff typically checks the patient's reported insurance coverage before the visit.
After an insured patient receives treatment for a given condition and supplies any applicable copayment, a healthcare provider or coder categorizes the nature of the treatment using codes according to the International Classification of Diseases, 10th Revision (ICD-10). The hospital or care facility then sends the care summary with ICD-10 and Current Procedural Technology codes to the patient's insurance company to see what portion of the care will be covered by insurance, with the patient billed for the remainder.
Benefits of revenue cycle management (RCM) and RCM systems
Proper RCM enables hospitals and other healthcare organizations to efficiently manage all functions associated with revenue generation. These functions might be administrative or clinical, and managing them makes it easier to identify and collect revenues from the patient services delivered.
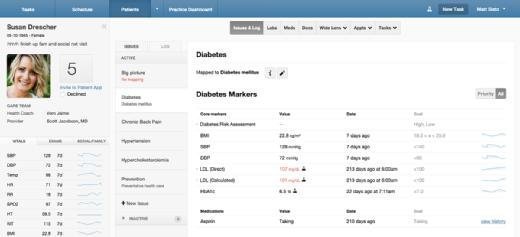
An RCM system is essential to store and manage patients' billing records, which in turn are essential for efficient and error-free revenue cycle management. Many vendors develop RCM systems, either as standalone products or integrated with electronic health record (EHR) systems, including GE Healthcare, Accenture, Experian Health, Cerner and Optum360.
An effective RCM system can reduce the amount of time that lapses between providing a service to a patient and receiving their payment by interacting with other health IT systems -- such as EHR and medical billing systems -- as patients move through the care process.
An RCM system can also save time by automating duties, such as administrative tasks, that were previously handled by employees. Examples of such tasks include informing patients of upcoming appointments, reminding payers and patients of an existing balance and reaching out to insurers with specific questions when a claim is denied.
An RCM system can also save providers money by providing insights into why claims have been denied. It can also prompt healthcare employees to enter all the information required for claims processing, which not only saves them from having to revise or resubmit claims, but also minimizes the probability of denied claims and gives providers better insight into why certain claims have been denied, thereby enabling them to rectify the issue. This also ensures that providers are reimbursed properly for treating Medicare patients.
Some RCM systems incorporate data analytics capability and provide dashboards to set and monitor revenue goals. The organization can also visualize opportunities for improving the revenue cycle by sorting billing data and reviewing corresponding reports. Today's advanced systems also include technologies such as cognitive computing to help ensure the correct medical codes are assigned to the correct patient, and robotic process automation to help speed up the process and optimize the overall revenue cycle.
Revenue cycle management and value-based care
RCM systems facilitate the healthcare industry's transition from fee-for-service to value-based reimbursement. The systems provide analytics that enable organizations to assess their patient population, see what portion of the population is suffering from which chronic diseases, monitor claims data and pinpoint any abnormalities. They can also provide reports about healthcare costs and patient satisfaction to insurers, increasing the chances of receiving full reimbursement from payers and minimizing the chances of claim denials.
Integrating RCM and clinical workflows through a customized EHR implementation can help a healthcare practice streamline efficiencies. See how a customized EHR implementation with RCM boosted a practice's growth.


