What is precision medicine (PM)?
Precision medicine (PM), also referred to as personalized or individualized medicine, continues to evolve as an important process in healthcare in which physicians and other caregivers develop treatments for patients based on genetic makeup, socioeconomic status and lifestyles. While the field typically examines human genomes and other factors for large groups of people with similar conditions, it can also be tailored to an individual patient's unique health requirements. The goal is to deliver the best healthcare -- be it medical procedures or prescription medications -- that is tailored to specific conditions.
The most common uses for precision medicine include cancer and diabetes treatments, cardiology and neurology applications, conditions related to aging, infectious diseases and rare illnesses.
History of precision medicine
While the concept of precision medicine seems to be a recent phenomenon, its roots go back centuries.
- 460-370 BC. Ancient Greek physician Hippocrates developed the concept of tailoring treatments to individual patients.
- 1901. Immunologist Karl Landsteiner developed the ABO grouping system, which helped formulate individualized treatments for patients based on blood type.
- 1953. Much of precision medicine is based on knowledge of genes and DNA structure discovered by molecular biologists James D. Watson and Francis Crick.
Precision medicine continues to progress with advances in genetic research and genomics -- especially DNA sequencing -- spurred by the Human Genome Project, which was completed in 2003. Since then, the use of data analytics, AI and cognitive computing in the health IT sector has supported its growth.
Two important government actions, both occurring in 2015, include the Precision Medicine Initiative (PMI) and the All of Us Research Program. The former has provided funding for cancer research using genomics, while the latter has been gathering data from a diverse population of individuals to support research activities. Additionally, the 21st Century Cures Act (2016) has provided funding for precision medicine research and product development.
This article is part of
AI in healthcare: A guide to improving patient care with AI
The following are among the most important recent and ongoing developments in precision medicine:
- Liquid biopsies that support cancer treatments. These tests gather genomic information (e.g., DNA) from bodily fluids and use the data to establish new alternatives to cancer care.
- Pharmacogenomics testing for mental and other health conditions. Data from pharmacogenomics tests may inform the development and focused delivery of drugs ideally suited to an individual.
- Linking therapy to genomic-based diagnostics. Based on the results of genetic testing, treatment programs can be more effectively tailored to specific user requirements.
- Predictive genetic tests. Results of such tests could provide more accurate predictions on the likelihood of a specific health issue occurring.
- Expansion of precision medicine. These might include research on large populations and their genetic attributes, the use of AI, the leveraging of genomics in routine clinical procedures, and how environments affect genetic testing.
- Technology developments. Developments in precision medicine will benefit from the use of specialized algorithms and the emergence of digital health applications based on genomics.
- Omics-based genomic sequencing. These technologies are based on knowledge of how an individual's entire genomic footprint affects their cells and bodily tissues.
Precision medicine vs. personalized medicine
Although the terms are sometimes used interchangeably and share similarities, differences exist between personalized medicine and precision medicine.
Personalized medicine is considered analogous to basic patient care, where healthcare providers make decisions about treatments based on what the patient needs or prefers. This is what makes the treatment "personalized."
By contrast, precision medicine describes medical therapies that are determined by analyzing specific subgroups of patients using factors such as genetics, family history, lifestyle and environment.
Putting both into perspective, results of precision medicine initiatives (e.g., medications, procedures and therapies) can be used as part of an individual's or a group's personalized medicine programs.
How do people benefit from precision medicine?
One of the major benefits of precision medicine is that it uses a comprehensive profile of the patient to determine an appropriate treatment. This includes not just genetics but family history, diet, exercise, stress level and more. These factors enable a healthcare provider to develop an effective treatment plan that is not based on the average patient, but rather on the individual patient.
By taking this approach, caregivers hope to increase the chances of patients surviving diseases such as cancer, which has dozens of variations. Much of today's efforts in cancer research, for example, focus on genetic characteristics of people and how variations in genes might spur the development of cancer cells.
Risks and concerns of precision medicine
Despite advances in medical technology and patient treatment based on precision medicine, several risks and concerns must still be addressed, both from provider and patient perspectives.
Provider perspective
Providers include medical professionals that deliver treatment to patients, pharmaceutical firms that develop drugs, firms that develop medical technology such as X-ray and CAT scan systems, and insurance companies as well as government agencies (e.g., Medicare and Medicaid) that reimburse for medical activities. The following are primary risks and concerns of precision medicine from a provider perspective:
- Quality and availability of data being used. Data quality and availability are increasingly important in all aspects of precision medicine to ensure that developed technologies and treatments are valid and effective.
- Managing costs associated with precision medicine. Tailoring and personalizing medical care increases costs for all kinds of healthcare providers, including personnel and resources.
- Regulatory and legislative compliance. Providers must deal with various federal government agencies, such as the FDA, NIH, CDC and CMS, ensuring they comply with the many different rules and legislation (e.g., HIPAA) related to the healthcare industry.
- Potential legal consequences. Unfavorable outcomes from the use of PM techniques might result in patient litigation.
Patient perspective
A satisfactory outcome is the primary goal for patients, regardless of the illness and treatment(s) used. The following are among the key patient risks and concerns regarding precision medicine:
- Privacy and security of patient data.
- Economic impact on patients.
- Potential harm from precision medicine.
- Limited access to precision medicine resources.
- Limited access to relevant clinical trials.
- Need for informed consent regarding how patient data will be used.
- Communicating findings from precision medicine activities.
- Potential discrimination based on how precision medicine is delivered.
- Psychological impact from knowledge of precision medicine findings.
- Inaccurate diagnoses or use of medicines.
- Loss of life or significant degradation of health.
- Changes in the dynamics of doctor-patient relationships.
Which government agencies address precision medicine?
The following government agencies are at the forefront of regulating and facilitating the continued development of precision medicine:
- Food and Drug Administration. The FDA provides oversight and support for precision medicine through its regulation of medical devices, therapies and diagnostic processes and tools. Among its many activities are supporting next-generation sequencing tests and reviewing as well as approving treatments for individual genetic profiles.
- National Institutes of Health. Research and development initiatives in precision medicine are supported by the NIH. As noted earlier, the All of Us Research Program, supported by the NIH, collects and processes data that is used to improve patient healthcare treatments.
- Centers for Medicare & Medicaid Services. Considering the costs associated with precision medicine and treatments, the CMS promulgates regulations governing how procedures are reimbursed and ensures that such treatments are available to patients.
- Centers for Disease Control and Prevention. Developments in precision medicine are supported by the CDC, ensuring that public health benefits from precision medicine through activities including genetic testing and strategies for disease prevention.
Similar organizations at state and local levels, along with many organizations focused on precision medicine, collaborate regularly with federal agencies.
Technologies used in precision medicine
Technology plays an increasing role in precision medicine. Here is a brief list of technologies used:
- Next-generation genomic sequencing. This technology generates a detailed analysis of a patient's genetic profile and delineates mutations or markers that can be used to identify disease and recommend treatment.
- Use of biomarkers. Proteins and genetic variations are defined as biomarkers that can predict disease risks and probable responses to medications and therapies.
- Omics technologies. These help analyze DNA, RNA, proteins and metabolites, along with their role in diseases.
- Electronic digital health devices. These can include devices a patient wears (e.g., a smartwatch) and mobile apps, both of which continually collect health data that can be used for patient diagnoses and treatments.
- Artificial intelligence. Many technologies in precision medicine use AI for tasks such as analyzing large data sets to discover patterns, forecasting possible outcomes and delivering guidance on patient treatment.
- Advanced imaging. Powerful digital technologies, such as molecular imaging, provide visual evidence of disease progression and treatment efficacy.
- Health IT systems. Technology platforms that collect and analyze vast amounts of data generate important outputs for precision medicine.
Vendors in precision medicine
Organizations leading the way forward in precision medicine include the following:
- Abbott Laboratories. This medical device manufacturer offers advanced diagnostic tools for precision medicine.
- Alnylam Pharmaceuticals. This biopharmaceutical company focuses on RNA-based therapies and treatment of rare genetic disorders.
- Illumina, Inc. This biotechnology firm offers integrated genomic sequencing systems.
- Novartis. In addition to pharmaceuticals, Novartis develops focused therapies and individualized treatments.
- Pfizer. Along with producing and distributing vaccines worldwide, Pfizer helps improve precision medicine with advanced drug development.
- Roche Diagnostics. This medical manufacturer delivers molecular diagnostics and PM technologies.
- Thermo Fisher Scientific. The clinical research company offers next-generation sequencing tools and genetic testing platforms.
- 2bPrecise. This PM data delivery company develops systems that integrate genomic data into electronic health records to facilitate decision-making.
The future of precision medicine
Rapid advancements in technology and government regulations that encourage the growth and use of precision medicine all contribute to a promising future. Here are some key trends in technology and research expected to drive this evolution:
- Artificial intelligence. AI is expected to unlock and augment advancements and improve patient outcomes.
- Advancement in gene and cell therapies. Continued development of therapies such as CRISPR (clustered regularly interspaced short palindromic repeats) and CAR (chimeric antigen receptor) T-cell address rare and complex diseases.
- Expanded use cases. The application of precision medicine for autoimmune and infectious diseases will increase alongside the development of oncology treatments.
- Impact on public health. Improvements in public health strategies are likely to emerge through precision medicine.
- Addressing ethical and regulatory concerns. As the benefits of precision medicine become available to more people, efforts to protect data privacy and ensure access to resources must also be addressed.
- Global collaboration. Growth of precision medicine will be increasingly supported through global partnerships and collaborations that share data, experience and innovation worldwide.
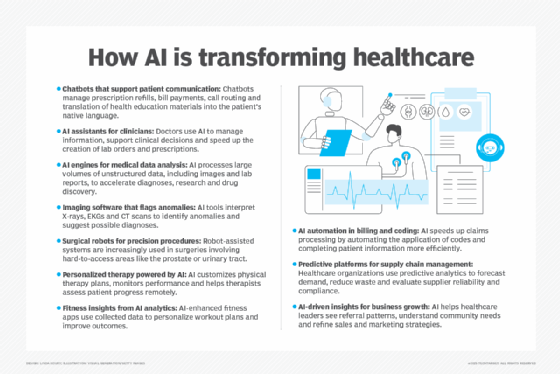
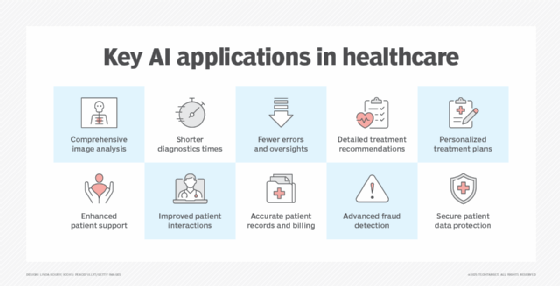
Healthcare was one of the first notable industries to achieve tangible AI benefits, including image analysis, accurate diagnoses, earlier treatments and patient privacy. Learn more about the benefits of AI in healthcare.






