clinical decision support system (CDSS)
What is a clinical decision support system (CDSS)?
A clinical decision support system (CDSS) is an application that analyzes data to help healthcare providers make decisions and improve patient care. It is a variation of the decision support system (DSS) commonly used to support business management.
What is the purpose of a CDSS?
A CDSS focuses on using knowledge management to get clinical advice based on multiple factors of patient-related data. Its purpose is to assist clinicians and healthcare providers in analyzing patient data and using that information for formulating a diagnosis and developing a treatment plan. Ultimately, the information provided enables them to improve the quality of the care their patients receive.
After analyzing a patient's information, a CDSS can make suggestions on drug doses and frequencies, and perform drug allergy checks. It might also provide guidelines and reminders regarding corollary prescription orders, such as glucose testing to coincide with an order for insulin.
Clinical decision support systems enable integrated workflows, provide assistance at the time of care and offer care plan recommendations. CDSS tools also offer reminders for preventive care, give alerts about potentially dangerous drug interactions and note when a patient has been scheduled to undergo tests that are possibly redundant. As such, using a CDSS can lower costs and increase efficiency. Also, eliminating unnecessary testing can help enhance patient safety and prevent potentially dangerous and costly complications.
Some providers deploy a CDSS to flag patients who were improperly diagnosed or might have missed a prescribed medication or were given the wrong dosage of a medication. These errors are added to problem lists and are included in population health management (PHM) reports that can serve as the basis for improvement initiatives.
When using a CDSS, data mining might be conducted to examine a patient's medical history in conjunction with relevant clinical research. Such analysis can then help predict potential events, such as drug interactions, or flag disease symptoms. That said, some physicians prefer to avoid over-reliance on their CDSS, preferring to rely on their professional experience to determine the best course of care.
Clinical decision support system and HITECH
The use of clinical decision support systems in the U.S. increased after the Health Information Technology for Economic and Clinical Health Act (HITECH Act) was passed. It stipulated that providers had to demonstrate the meaningful use of health IT by 2015 or face a reduction in Medicare reimbursements the following year.
Under meaningful use, providers must implement one clinical decision support rule, including diagnostic test ordering and the ability to track compliance with that rule. That rule, furthermore, should apply to a specialty or high-priority condition. HITECH's stage 2 standards for meaningful use incorporate the area of clinical decision support. By mandating the integration of a CDSS into medical records as part of the meaningful use legislation, HITECH aims to ensure that physicians have up-to-date medical knowledge and evidence-based guidance at the point of care.
What are the main types of CDSS?
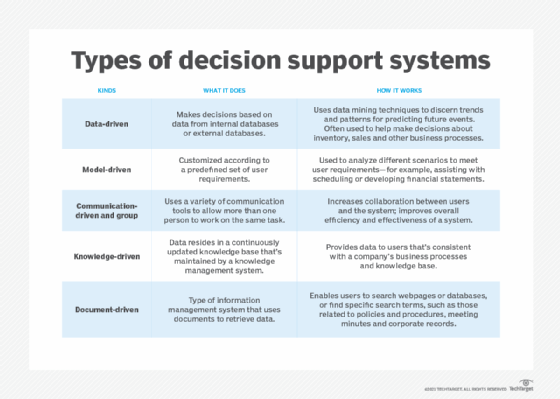
There are two main types of CDSS.
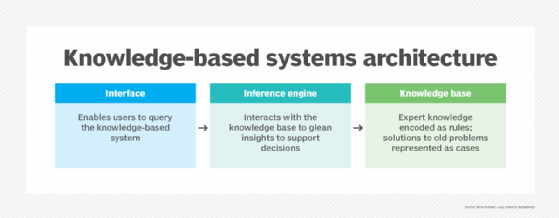
A CDSS that uses a knowledge base applies rules to patient data using an inference engine and then displays the results. Most knowledge-based systems consist of a data repository, an inference engine and a mechanism to communicate. Also, these systems commonly operate under if-then rules. For example, to assess potential drug interactions a rule might be that if drug A is taken and drug B is prescribed, then an alert should be issued.
The other type of CDSS relies on machine learning or statistical pattern recognition to analyze clinical data. An example of a non-knowledge-based CDSS is an artificial neural network, which learns how to perform certain tasks by considering specific examples, usually without being programmed with if-then or other task-specific rules. The neural network discovers and analyzes patterns found in patient data to determine relationships between symptoms and a diagnosis.
Computerized physician order entry and electronic health records with CDSS
Computerized physician order entry (CPOE) refers to a variety of systems used to automate the medication ordering process. CPOEs ensure legible, complete orders by only accepting them in a standardized format. A CPOE can interface with a CDSS to further enhance the efficacy and safety of patient care.
Clinical decision support systems and electronic health records (EHRs) are often integrated to streamline workflows and make use of existing data sets. A growing number of CDSS functions are built into EHR systems.
Drawbacks of a CDSS
There are some drawbacks to clinical decision support systems.
A CDSS must integrate with a healthcare organization's clinical workflow, which is often already complex and made even more so by the integration.
Some clinical decision support systems are standalone products that lack interoperability with reporting and EHR software, limiting their usefulness in clinical and administrative settings. Also, the number of clinical research and medical trials being published on an ongoing basis makes it difficult to incorporate the resulting data into a CDSS in a timely manner. Incorporating large amounts of data into existing systems places a significant strain on application and infrastructure maintenance.
Another potential problem with a CDSS is alert fatigue. The alerts triggered by a CDSS can overwhelm caregivers who also receive prompts from other technology systems. As a result, they might ignore one or more alerts, which might have significant consequences for diagnosis, decision-making and other patient care activities.
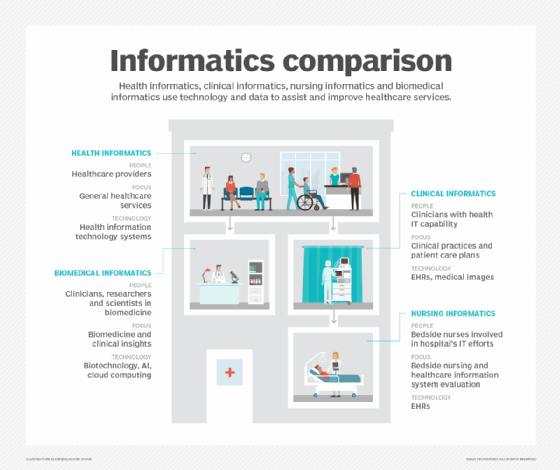
Learn how primary care electronic health record (EHR) integration enhances social determinants of health documentation. Explore why medical specialty societies are key to advancing health data standards. See what role EHRs play in clinical informatics and how health information exchanges can support public health and equity.






