What is population health management (PHM)?
Population health management (PHM) is a data-driven discipline within the healthcare industry that seeks to improve health outcomes for a defined population. Unlike public health management initiatives that focus on improving the health of an entire population, population health management initiatives target a subgroup within a healthcare system or insurance network. Each subgroup is clearly defined so that relevant data can be collected and used in a consistent manner.
PHM initiatives proactively address the healthcare needs of a defined population more efficiently at both the group (cohort) and individual level by using data-driven insights and coordinating care across providers. Technology enables PHM teams to aggregate healthcare data from disparate sources, analyze the data holistically and use the results to manage a specific healthcare population and its members at scale.
From a financial standpoint, population health management (PHM) supports value-based care (VBC) by helping providers lower costs while improving the quality of care. In recent years, advancements in artificial intelligence (AI) have made it easier to align clinical data with risk, utilization, cost and outcomes data. The improved alignment is helping providers make evidence-based decisions more efficiently and meet VBC targets across multiple care settings more effectively.
Population health management goals
The primary goal of population health management is to improve the overall health outcomes of a defined group while making healthcare delivery more efficient and cost-effective. Data-driven insights are used to assign risk levels, flag care gaps and support targeted interventions in a proactive, rather than reactive, manner. The shift from reactive to proactive care enables providers to anticipate the need for interventions earlier, reduce preventable hospitalizations, and consistently deliver quality outcomes.
It should be noted that a PHM program's success often depends on how actively patients participate in their own care. While PHM teams can use data, analytics and care coordination strategies to create evidence-based action plans, high patient engagement ensures healthcare plans get followed over time. This is why another important goal of PHM is to help identify and address potential social determinants of health (SDOH) within a population group. SDOH factors are non-medical factors that influence patient well-being. Important SDOH factors include housing stability, food security, transportation access and employment.
SDOH factors play an important part in PHM because they often have as much (or more) affect on health outcomes as clinical care factors. To quantify SDOH risk levels so they can be included in PHM data analytics, providers often use standardized screening tools such as the PRAPARE questionnaire or the Accountable Health Communities (AHS) health-related social needs (HRSN) questionnaire. Once social risks have been identified, PHM teams can act on the insights by connecting patients with housing assistance programs, partnering with food banks to reduce food insecurity, coordinating with transportation services to ensure patients can attend medical appointments or referring individuals to job training and financial counseling services.
Population health management and risk stratification
In the context of population health management, risk stratification is a process that assigns each person in a defined population one or more risk levels based on their medical history, current health status, SDOH factors and predicted need for healthcare services in the future.
Stratification workflows use machine learning algorithms and data from electronic health records (EHRs) and insurance claims -- as well as data from pharmacy records, lab results and social screenings -- to assign patients to low, rising or high risk categories. The objective is to identify which members of a defined population are healthy, which members may be developing health problems and which require the most care.
Risk stratification is important because it helps healthcare providers understand a defined population. Once a population has been stratified, it becomes easier for a PHM team to match levels of care with levels of need. For example, a low-risk patient might be given access to educational resources, while a rising-risk patient might be referred to a disease management program for closer monitoring and preventive support.
How population health management works
Population health management initiatives begin by identifying a specific group whose health will be monitored and improved. For example, a targeted population might be all patients in a healthcare network, all network members with the same insurance plan, or all individuals with the same health-related concern. Once a group has been identified, data is collected from multiple sources to provide a complete picture of each person's health status and create a baseline assessment of the population's overall needs.
The next step is to analyze the aggregated data and identify patterns that can be used to assign risk levels and/or discover gaps in care. Care coordination is an important part of this workflow because it ensures people and processes have access to the same information and outcomes are measured in the same way. This consistency helps reduce duplication, prevent errors and ensure interventions are evidence-based and aligned with value-based care goals.
After care coordination is established, targeted interventions can be implemented based on the insights gained from risk stratification and care gap analysis. Patient engagement becomes a priority during this phase. Tools like patient portals, mobile health apps and health coaching programs can help individuals stay informed, follow treatment plans and adopt healthier lifestyle habits. Healthcare teams can monitor outcomes and adjust recommendations as needed throughout the process. If the results aren't meeting targets, care strategies can be adjusted, resources can be reallocated, and new interventions can be tested.
Artificial intelligence is increasingly making it easier for healthcare organizations to identify risks, personalize care and operate more efficiently and cost-effectively. For example, an AI-enabled PHM platform can flag patients who are at higher risk of developing diabetes, highlight care gaps for specific patients who have already been diagnosed with diabetes and predict which diabetic patients are most likely to be admitted to the hospital in the next six months. When care teams have easy access to this type of information, they can intervene earlier with more precision and improve outcomes for the population cohort at both group and individual levels.
The benefits of population health management
PHM can help healthcare organizations create better outcomes and reduce healthcare costs by:
- Identifying medical risks earlier;
- Helping care teams provide evidence-based interventions and care plans more efficiently;
- Eliminating unnecessary or duplicate healthcare services;
- Improving outcomes by engaging patients as active partners.
Another major benefit of PHM is that it supports the Institute for Healthcare Improvement (IHI) Triple Aim framework. The Triple Aim framework is widely used to improve population health, improve patient experience and reduce per capita healthcare costs. Technology provides the tools that make reaching those goals realistic at scale.
Population health management technologies and tools
Technology and software tools make it easier for care teams to collect, analyze and act on healthcare data in real time. Arguably, electronic health record systems provide the most well-rounded view of patient health when they can store both clinical and SDOH data. The integration provides a more comprehensive health profile for each patient and makes it easier to compile a complete data set for population analysis.
Other tools and technology used to deliver proactive, value-based care for a defined population include:
Data aggregation platforms
This type of platform can gather data from disparate sources and provide a unified view that data analytics platforms can use to improve patient care, operational efficiency and financial outcomes.
SDOH screening tools
Social determinants of health screening tools can be used to capture additional information about economic and social factors that affect population health.
Healthcare analytics platforms
This type of software platform leverages various technologies, including machine learning, to identify data patterns, predict risks and segment large populations into smaller cohorts.
Clinical decision support systems
Clinical decision support systems provide evidence-based recommendations to guide providers in diagnosis and treatment.
Predictive modeling
Predictive modeling tools use healthcare data to forecast events like hospital readmissions or medication nonadherence.
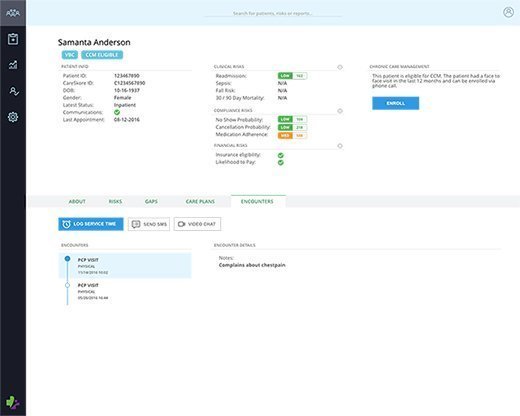
Care management software
Care management and case management software platforms allow providers to create personalized care plans, track patient progress and communicate with patients outside clinical settings.
Patient engagement tools
Patient engagement tools such as wearable medical devices and mobile health apps can help individuals monitor their health more effectively by sending reminders or alerts.
Health information exchanges
Health information exchanges (HIEs) facilitate secure data sharing between healthcare organizations and help ensure all providers involved in a patient's care have access to the same information.
Telehealth platforms
Telehealth platforms can facilitate patient/provider communication over the internet and make supporting specific population groups in remote and/or underserved locations easier.
Population health management software
Hospitals, local healthcare providers, accountable care organizations (ACOs) and payers can implement PHM software on-premises or in the cloud. Here's a short list of leading PHM software platforms and their key features:
Athenahealth
- Allows care teams to identify high- and rising-risk patients easily.
- Supports seamless PHM across multiple EHRs for populations of any size.
- Provides dashboard and reporting functionalities that show cost and utilization trends across a defined population.
Epic Healthy Planet
- Promotes patient wellness with integrated EHR and social care tools.
- Supports data aggregation, risk stratification, care gap tracking and quality measure reporting.
- Includes built-in patient outreach and engagement tools.
Oracle Health Data Intelligence
- Cloud-based platform that can pull data from multiple EHRs and external systems.
- Offers predictive analytics, SDOH integration and customizable dashboards.
- Supports care coordination across diverse provider networks.
Philips Wellcentive
- Known for its robust data aggregation and normalization capabilities.
- Includes predictive analytics, quality program reporting, and patient outreach functions.
- Targets value-based care programs and ACO performance.
Innovaccer Health Cloud
- Strong emphasis on interoperability and SDOH integration.
- Offers advanced analytics, care management workflows and real-time performance tracking.
- Provides AI-driven insights and customizable reporting.
Azara Healthcare
- Enables insight into risk factors for population health.
- Provides strong support for value-based care.
- Allows healthcare organizations to identify appropriate interventions and close critical care gaps.
Conifer Health Solutions
- Promotes an understanding of common health risks and trends among employees.
- Identifies health risks, implements preventive measures and supports individuals in managing chronic conditions.
- Encourages screenings, vaccinations and healthy habits.
Arcadia
- Offers customized workflows.
- Known for realistic healthcare benchmarks.
- Provides metrics for evaluating how efforts measure up in niche groups or the broader population.
Learn more about the data interoperability issues in healthcare that still exist despite recent efforts to promote seamless data sharing across healthcare systems.






