ICD-10-CM (Clinical Modification)
What is ICD-10-CM (Clinical Modification)?
The ICD-10-CM (International Classification of Diseases, Tenth Revision, Clinical Modification) is a system used by physicians and other healthcare providers to classify and code all diagnoses, symptoms and procedures related to inpatient and outpatient medical care in the United States. It provides a level of detail that is necessary for diagnostic specificity and morbidity classification in the U.S.
Like its predecessor, ICD-9-CM, ICD-10-CM is based on the International Classification of Diseases (ICD), which is owned and published by the World Health Organization (WHO). ICD-10-CM uses unique alphanumeric codes to identify diseases, injuries and other healthcare-related information.
The ICD-10-CM codes are used daily by a wide range of individuals to store and retrieve diagnostic information. This includes physicians, nurses, medical coders, IT professionals, insurance agents, managers and others who work with medical data. The codes are also used in the compilation of national mortality and morbidity statistics.
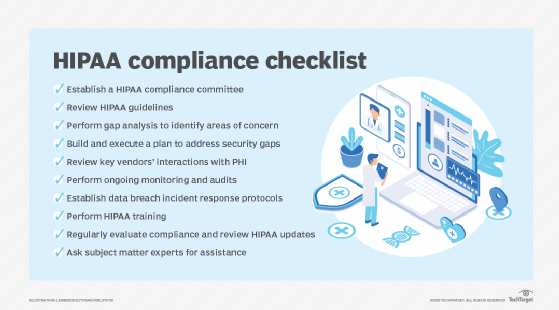
The National Center for Health Statistics (NCHS) is the U.S. federal agency responsible for the use of ICD-10-CM in the U.S. The NCHS is part of the Centers for Disease Control and Prevention (CDC), which is one of the main operating divisions of the Department of Health and Human Services (HHS). The HHS has mandated that all entities covered by the Health Insurance Portability and Accountability Act (HIPAA) must adhere to ICD-10-CM codes. The mandate went into effect on October 1, 2015.
Importance of ICD-10-CM codes
ICD-10-CM replaced volumes 1 and 2 of ICD-9-CM, offering a number of improvements over its predecessor. ICD-10-CM also enhanced ICD-10 in various ways to meet the specific needs of U.S. healthcare.
ICD-10-CM provides greater specificity in code assignments than ICD-9-CM, defining nearly five times more diagnostic codes. It also offers more information about the severity of a patient's condition, as well as details relevant to ambulatory and managed care. In addition, ICD-10-CM adds combination diagnosis/symptom codes, reducing the number of codes needed to describe a condition.
The U.S. started using ICD-9-CM for morbidity data in 1979, so the move to ICD-10-CM was long overdue. Most developed countries had already transitioned to ICD-10, and it was becoming increasingly difficult to compare morbidity data at an international level. In some cases, ICD-9-CM was no longer clinically accurate, and it was running out of code capacity to expand, as most of the code categories were completely full. Additionally, ICD-9-CM codes lacked the specificity and detail provided by ICD-10-CM.
The NCHS began working on ICD-10-CM in the 1990s, after it was endorsed in May 1990 by the 43rd World Health Assembly (WHA). From December 1997 through February 1998, the NCHS made a draft of ICD-10-CM available for public comment on its website. After reviewing the comments, the NCHS made additional modifications to ICD-10-CM. In the meantime, the U.S. adopted ICD-10 for mortality coding and classification in 1999.
The NCHS continued to work on ICD-10-CM, which focused on morbidity coding and classification. In 2003, the American Hospital Association (AHA) and the American Health Information Management Association (AHIMA) field-tested ICD-10-CM. The NCHS then incorporated the modifications that came out of this effort. However, it wasn't until 2015 that the U.S. officially finally adopted ICD-10-CM for morbidity coding and classification.
ICD-10-CM format
The NCHS and the Centers for Medicare and Medicaid Services (CMS) now oversee all changes and modifications to the ICD-10-CM, with updates released annually. The most current version is FY2024, which applies to discharges and other patient encounters from October 1, 2023, through September 30, 2024. This FY2024 release, like previous ICD-10-CM releases, is divided into two main parts:
- Alphabetic Index. Alphabetical list of the terms and their corresponding codes. The index is divided into four parts: Index to Diseases and Injury, External Cause of Injuries Index, Table of Neoplasms, and Table of Drugs and Chemicals.
- Tabular List. Hierarchical list of all the categories, subcategories and their diagnoses, organized around the code structure. The categories are divided into chapters based on diseases, disorders and other conditions.
In addition to the Alphabetic Index and Tabular List, the NCHS and CMS provide a set of guidelines for working with ICD-10-CM codes. The guidelines for the FY2024 release were approved by the four organizations that comprise the Cooperating Parties for ICD-10-CM: CMS, NCHS, AHA and AHIMA.
The guidelines were developed as a companion resource to the Alphabetic Index and Tabular List and apply to all healthcare settings unless otherwise noted. The guidelines are organized into the following four sections:
- Section I: Conventions, general coding guidelines and chapter-specific guidelines.
- Section II: Selection of Principal Diagnosis (non-outpatient settings).
- Section III: Reporting Additional Diagnoses (non-outpatient settings).
- Section IV: Diagnostic Coding and Reporting Guidelines for Outpatient Services.
Code structure
ICD-10-CM codes follow a specific structure:
- The codes use alphanumeric characters. The alphabetic characters are not case-sensitive.
- Each code is between three and seven characters.
- The first character is always alphabetic and can be any letter except U.
- The second character is always numeric.
- The remaining characters can be either alphabetic or numeric.
- If a code contains more than three characters, a period follows the third character.
The codes are defined in hierarchical order, with categories at the top of the hierarchy and subcategories beneath them. The code used for a diagnosis is the one at the lowest level of any specific branch. However, the categories and subcategories can have different levels of granularity, so what constitutes the diagnosis code will depend on the breakdown of the individual category and its subcategories.
Each category code is three characters, and each subcategory code is either four or five characters. A subcategory might include elements beneath it, in which case, those elements or their children elements are used for the diagnosis codes. If a subcategory does not have any child elements, the subcategory is considered the lowest level of that particular branch, in which case, it is used as the diagnostic code. The final level of any branch is the diagnostic code.
To illustrate how this works, consider the category "D81 Combined immunodeficiencies." (The code in this case is D81.) The category contains multiple subcategories, including "D81.8 Other combined immunodeficiencies." This subcategory includes three of its own entities:
- D81.81 Biotin-dependent carboxylase deficiency.
- D81.82 Activated Phosphoinositide 3-kinase Delta Syndrome [APDS].
- D81.89 Other combined immunodeficiencies.
D81.82 and D81.89 do not contain any of their own entities, which means that they're at the final level of their branch within the code hierarchy. As such, they're used for the diagnostic codes. However, D81.81 is further subdivided, so it is not considered the lowest level. D81.81 contains the following three entities:
- D81.810 Biotinidase deficiency.
- D81.818 Other biotin-dependent carboxylase deficiency.
- D81.819 Biotin-dependent carboxylase deficiency, unspecified.
In this case, these three codes represent the most granular level for subcategory D81.81, because they have not been further subdivided.
CMS guidelines state that diagnosis codes should be used and reported at the highest number of available characters, that is, at their most granular levels. Three-character codes should be used only if they are not further subdivided. A code is considered invalid if it has not been coded to the deepest level possible.
Some categories require a special seventh character that further qualifies the elements within that category. For example, the subcategory "M48.4 Fatigue fracture of vertebra" includes multiple elements that further subdivide the category into diagnostic codes. The subcategory also states that each diagnostic code requires one of the following digits for the seventh character:
- A -- initial encounter for fracture.
- D -- subsequent encounter for fracture with routine healing.
- G -- subsequent encounter for fracture with delayed healing.
- S -- sequela of fracture.
When a category requires the use of the seventh character, all codes within that category must use the seventh character. If the code contains fewer than six characters, the special seventh character must still be included, in which case, a placeholder X should be used for the missing characters. For example, if code M48.41 should include a G as the seventh character, it would be written as M48.41XG. The ICD-10-CM standard also uses X as a placeholder for certain codes to allow for future expansion.
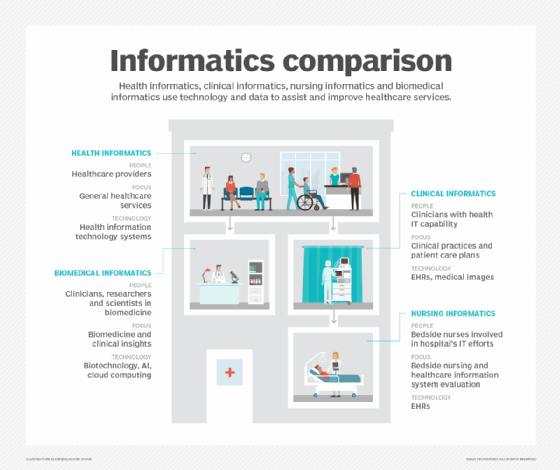
Learn the four levels of health data interoperability outlined by the Healthcare Information and Management Systems Society (HIMSS) and see why medical specialty societies are key to advancing health data standards. Explore what role EHRs play in clinical informatics and how health information exchanges can support public health and equity.





