ICD-10 (International Classification of Diseases, 10th Revision)
What is ICD-10 (International Classification of Diseases, 10th Revision)?
The International Classification of Diseases, 10th Revision (ICD-10), is a global standard for classifying and coding mortality and morbidity data. The U.S. adopted ICD-10 for mortality coding on death certificates in 1999. Sixteen years later, the U.S. adopted ICD-10 for morbidity, but did so indirectly by creating its own standards based on the ICD-10 codes. The U.S. standards became effective on Oct. 1, 2015.
ICD-10 is an update to ICD-9. ICD-10 takes into account modern advances in clinical treatment and medical devices, and it offers more classification options than ICD-9. The World Health Organization (WHO) owns, develops and publishes the ICD codes. National governments and other regulating bodies adopt them into their own systems. WHO publishes minor updates every year and major updates every three years.
ICD-10 purpose and uses
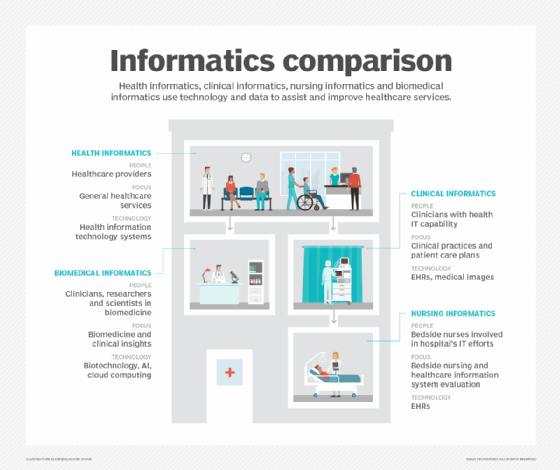
Within the healthcare industry, health providers, insurance carriers, government agencies and other organizations use ICD codes to specify diseases on health records, track epidemiological trends and assist in medical reimbursements. A wide range of individuals use these codes daily, including physicians, nurses, managers, medical coders, IT professionals, insurance agents and many others.
The ICD provides an international system for classifying and coding diseases, disorders, injuries and other health conditions. By standardizing this information, the ICD makes it easier to store, retrieve and analyze health data. It also enables organizations to share health information, compare health data across sectors or time, and make evidence-based decisions.
The ICD classifications and codes are also used for clinical research and to monitor the incidence and prevalence of death, disease, symptoms, injuries and other health-related events. In addition, the ICD can help in observing resource allocation trends, as well as in tracking safety and quality guidelines.
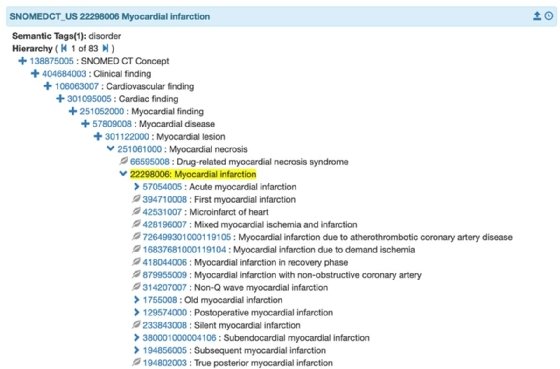
ICD-10 is sometimes used in conjunction with Systematized Nomenclature of Medicine -- Clinical Terms (SNOMED CT), a multilingual vocabulary of clinical terminology that is used to capture the clinical data of a care episode. Mapping SNOMED CT to ICD-10 can help simplify reporting and access to medical information, as well as enable computer-assisted coding systems that improve the accuracy, efficiency and consistency of coding. The mapping can also show how a healthcare provider approached a medical procedure and what type of medical device was used.
The history of ICD-10 in the U.S.
Work on ICD-10 first began in 1983 and was endorsed by the 43rd World Health Assembly (WHA) in May 1990. Some countries began using ICD-10 codes in 1994. The U.S. adopted the standard for its own mortality coding in 1999, but continued to use ICD-9 for morbidity coding until 2015. The U.S. had been using ICD-9 since 1979 and was one of the last developed countries to adopt the revision.
Supporters of ICD-10 claimed that ICD-9 had become obsolete, didn't account for modern healthcare practices, and lacked ICD-10's specificity for clinical diagnoses and medical device coding. After many delays, the U.S. finally adopted ICD-10 for morbidity coding, although they did not use the ICD-10 standard directly. Instead, two federal agencies created their own standards based on ICD-10:
- ICD-10 Clinical Modification (ICD-10-CM). The standard was developed by the U.S. National Center for Health Statistics (NCHS) for use in medical diagnosis. It replaced ICD-9-CM, volumes 1 and 2. ICD-10-CM added information specific to ambulatory and managed care, combined diagnostic and symptom codes, incorporated new subclassifications, and made other changes. ICD-10-CM currently includes about 78,000 codes.
- ICD-10 Procedure Coding System (ICD-10-PCS). The standard was developed by the U.S. Centers for Medicare and Medicaid Services (CMS) for classifying procedures performed in hospital inpatient settings. It replaced ICD-9-CM, volumes 3. The standard included support for data collection, payment and electronic health records. ICD-10-PCS currently includes over 78,000 codes.
The ICD-10-CM and ICD-10-PCS conform to WHO's ICD-10 layout, while allowing for additional details found in U.S. healthcare.
The transition to ICD-10
The ICD-10 conversion in the U.S. was delayed by lobbying, politics and general opposition to the increased amount of codes in the newer set. Physicians, in particular, opposed the new revision, with groups like the American Medical Association lamenting the cost of ICD-10 implementation and believing it would take away resources from other areas. Below is a brief timeline of events that eventually led to ICD-10 implementation:
- Jan. 16, 2009. The U.S. Department of Health and Human Services (HHS) published a final rule establishing ICD-10 as the new national coding standard for morbidity, with an adoption date of Oct. 1, 2013.
- Aug. 24, 2012. HHS announced a delay in ICD-10 adoption from Oct. 1, 2013, until Oct. 1, 2014, to allow healthcare systems more time to prepare for the transition.
- March 2013. At the 2013 meeting of the Healthcare Information and Management Systems Society (HIMSS), a CMS administrator said ICD-10 would not be delayed past Oct. 1, 2014.
- April 1, 2014. Then-President Barack Obama signed a Medicare reimbursement bill from Congress that included a delay in ICD-10 implementation from Oct. 1, 2014, until Oct. 1, 2015.
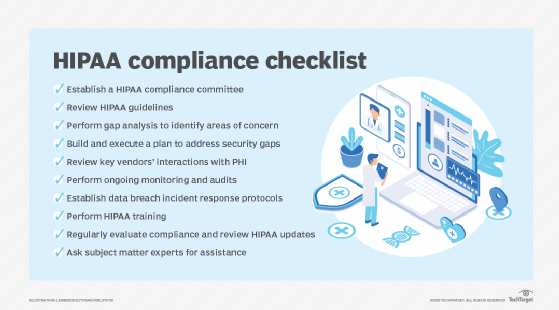
Once the ICD-10 codes were adopted, all entities covered under the Health Insurance Portability and Accountability Act (HIPAA) were required to transition to ICD-10. Entities not covered by HIPAA weren't required to transition, but they could still adopt the coding system, which could help entities such as automobile insurers and workers' compensation programs with injury classification and the coordination of benefits.
Why was transitioning to ICD-10 important?
When ICD-10 was introduced, it provided more detailed information for measuring healthcare quality, safety and efficacy than ICD-9. The more specific set of codes promised to improve the following processes:
- Value-based reimbursement.
- Outcome measurements.
- Clinical, financial and administrative performance measurement.
- Payment systems and claims processing.
- Reporting on new medical technology.
- Reimbursement systems.
- Care and disease process management.
The adoption of the ICD-10 codes also allowed for more accurate payment for new procedures, fewer rejected claims, fewer fraudulent claims, improved disease management and a better understanding of new procedures.
Key differences between ICD-9 and ICD-10
The ICD-10 codes greatly expand the classification options compared to ICD-9. For example, the initial ICD-10-CM included about 68,000 codes, as opposed to 13,000 in ICD-9-CM, according to the Centers for Medicare & Medicaid Services.
ICD-10 codes also include alphanumeric categories, while ICD-9 has only numeric categories. In addition, the ICD-9 codes are based on three to five letters and numbers, while the ICD-10 codes are based on three to seven letters and numbers. The seventh character was added to further specify a diagnosis, such as capturing data about the treatment phase, as follows:
- A (initial encounter). Although the name implies it is the patient's initial visit, initial encounter refers to the period during which the patient is receiving active treatment for a condition.
- D (subsequent encounter). Subsequent encounter refers to an encounter after the patient has received active treatment, during the recovery phase.
- S (sequela). Sequela refers to a complication or condition that is a direct result of an injury, such as a scar.
Furthermore, ICD-10 renames some titles, changes chapters, and groups certain conditions together. ICD-10 also provides more details about the patient's condition. For example, if a patient broke a wrist, ICD-9 did not specify whether it was the left or right wrist, but ICD-10 offers either option. ICD-10 also presents additional details on when a patient is seen by a caregiver and how an injury or disease is progressing or healing.
ICD-11 replaces ICD-10
ICD-10 is no longer the latest release of the ICD standard. In 2019, the World Health Assembly adopted ICD-11, which went into effect on Jan. 1, 2022. The ICD-11 revision incorporates input from over 90 countries and brings with it a number of improvements over ICD-10. It also clarifies terms, simplifies the coding structure and expands the overall scope.
ICD-11 is entirely digital, making it more usable in IT environments. It provides an application programming interface (API) as well as online and offline tools. In addition, it can integrate with electronic data sources and is presented in a more user-friendly format. The new release also reflects recent progress in medicine and scientific understanding. For example, codes specific to antimicrobial resistance are now aligned with the Global Antimicrobial Resistance Surveillance System.
ICD-11 also provides a wide range of other improvements, such as the following:
- Includes codes for the clinical stages of HIV.
- Updates diagnostic recommendations for mental health conditions.
- Adds digital documentation of COVID-19 certificates.
- Includes new chapters on sexual health and traditional (complementary) medicine.
- Internationalizes coding for traffic accidents and causes of injuries.
- Adds gaming disorder to the addictive disorders section.
- Includes codes for the full documentation of patient safety.
- Expands the sections on cancer, cardiology, dementia, diabetes, infectious diseases, and allergies and immune system disorders.
It is unclear when and how the U.S. will adopt ICD-11, but the National Committee on Vital and Health Statistics (NCVHS) is urging federal agencies to take an aggressive and proactive approach to the new standard and to avoid the protracted regulatory process that plagued ICD-10. The NCVHS makes several recommendations for moving forward on ICD-11 and believes that by following these recommendations, the U.S. can find a path forward that supports national healthcare priorities, while optimizing benefits and minimizing costs.
Learn how primary care electronic health record (EHR) integration enhances social determinants of health documentation. Explore the benefits of clinical documentation improvement and why medical specialty societies are key to advancing health data standards. See what role EHRs play in clinical informatics and how health information exchanges can support public health and equity.