What is health IT (health information technology)?
Health IT (health information technology) is the area of IT involving the design, development, creation, use and maintenance of information systems for the healthcare industry. Automated and interoperable healthcare information systems can improve medical care and public health, lower costs, increase efficiency, reduce errors, improve patient satisfaction and optimize reimbursement for healthcare providers.
Why is healthcare IT important?
Continuing advances and improvements in healthcare IT ensure that patients receive the best possible diagnoses, treatments, medications, surgical procedures and experiences within the healthcare industry. Health IT links the many different clinical systems with administrative and information services into a unified IT infrastructure. It also supports information sharing for surgeries and procedures, medical treatments and other areas of healthcare. By simplifying and streamlining healthcare delivery, health IT benefits patients, healthcare professionals and healthcare organizations alike.
Healthcare IT users include hospitals, outpatient centers, pharmaceutical companies, clinical laboratories, healthcare professionals and patients. Healthcare organizations depend on the availability of healthcare IT to support administrative, research, education and clinical activities. Patients increasingly use healthcare IT through telehealth services, which deliver remote interactions with healthcare providers.
Examples of health IT
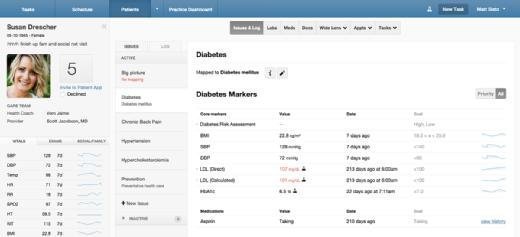
The electronic health record (EHR) is the central component of the health IT infrastructure. An EHR, or electronic medical record (EMR), is a person's official, digital health record shared among multiple healthcare providers and agencies. Other key elements of the health IT infrastructure are the personal health record (PHR), which is a person's self-maintained health record, and the health information exchange, a health data clearinghouse or a group of healthcare organizations that enter into an interoperability pact and agree to share data among their various health IT systems.
This article is part of
AI in healthcare: A guide to improving patient care with AI
In addition to patient records, technology is increasingly present in surgical and procedural areas. For example, robots assist orthopedic surgeons in hip, knee and shoulder replacements. With robotic technology, they can perform repetitive procedures the same way every time, delivering more consistent outcomes and enhancing safety by reducing the likelihood of human error.
Advances in smartphones and other mobile devices, such as smartwatches, network technology and the internet, extend healthcare IT to patients. PHR and EHR technology have become major components in healthcare today. As a result, concerns about protecting the security and availability of PHRs and EHRs have grown significantly.
The mountains of patient information that health IT generates have spurred the development and use of artificial intelligence (AI) technology to better manage and interpret that data. AI-powered data analytics are moving out of research settings and beginning to play a greater role in day-to-day clinical activities and operations. AI makes it easier to aggregate patient information, analyze it and then base diagnoses and treatments on the results. For example, AI algorithms can quickly and accurately analyze imaging results or detect early warning signs of disease.
Today's health IT technologies are components of many medical systems, such as picture archiving and communication systems and vendor-neutral archives. These systems store and manage patients' medical images. In addition to radiology, health IT technologies are increasingly used in other specialties, such as cardiology and neurology, which are also large-scale producers of clinical imaging.
Improvements in health technology include patient portals and telehealth services, which have gained near-ubiquitous adoption. These technologies let patients securely communicate with their care team, pay bills, check services against what an insurance plan allows, download medical records, make appointments, request prescription refills and interact with chatbots for other services.
Issues and developments in healthcare IT
Numerous U.S. government agencies and laws affect healthcare and, by extension, health IT:
- Health Insurance Portability and Accountability Act, or HIPAA.
- Health Information Technology for Economic and Clinical Health, or HITECH Act.
- Affordable Care Act.
- 21st Century Cures Act.
- Medicare Access and CHIP Reauthorization Act, or MACRA.
- Department of Health and Human Services.
- Centers for Medicare and Medicaid Services.
- Assistant Secretary for Technology Policy/Office of the National Coordinator for Health IT.
- Food and Drug Administration, or FDA.
State-level agencies and legislation regulate various aspects of health IT in the U.S.
HIPAA's security and privacy rules have long guided healthcare organizations in providing patients with access to their medical records while safeguarding that information. However, the need for more robust security has become more urgent in recent years as data breaches, malware and ransomware attacks have increased in frequency and severity.
In response, cybersecurity systems and procedures, incident response plans, data backup and recovery, and the use of cloud-based technologies augment traditional health IT systems. Employee education is also part of the solution, as human errors can lead to data breaches. Many healthcare organizations, for example, conduct routine phishing simulations and can track inappropriate access to electronic medical records.
From a workforce perspective, IT managers and chief information officers in healthcare organizations have risen in importance and authority as technology becomes more prevalent.
Another important discipline aligned with healthcare IT is health informatics, which uses health IT systems and data analysis to enhance care.
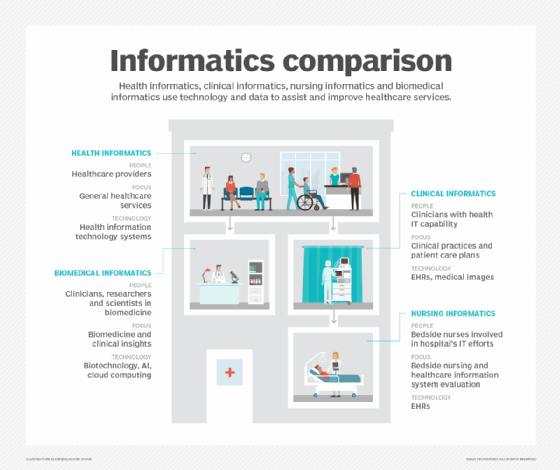
Informatics team members are interdisciplinary, usually comprising a mix of IT and clinical backgrounds. Their work combines science, medicine, nursing and IT to improve care, clinical documentation, patient safety, communication, resource utilization and more.
How does health IT improve healthcare?
The principal goal of healthcare IT is to help patients obtain the best possible outcomes by using technology to make care more efficient, effective and equitable.
Secure messaging apps enable clinical teams to communicate quickly and easily, even across multiple sites, contributing to safer care transitions. Data dashboards can help hospitals track bed and operating room utilization in real time, enabling them to identify potential issues with patient throughput. Surgical navigation systems combine high-resolution imaging with advanced software to enable surgeons to track instrument position with the utmost precision, leading to better outcomes. These are just a few examples of how health IT can improve healthcare.
More broadly, health IT can improve healthcare in the following ways:
- Data analytics and big data can guide population health programs and reduce the incidence of expensive chronic health conditions.
- Cognitive computing and analytics can inform precision medicine and personalized treatments.
- Academic researchers can share data to develop new diagnostic tools and therapies.
- Telemedicine technologies can improve clinician-patient interactions.
- Health informatics can enhance clinical decision support systems, which provide evidence-based recommendations at the point of care.
- EMR systems support patients' rights to access their health data and more easily participate in their care.
- AI can reduce the chances of errors in medications, medical procedures and diagnostic activities.
Although health IT has contributed to many innovations and advancements in healthcare, it has also created challenges. The importance of documenting patient data in EHRs has placed significant administrative burdens on frontline clinicians, often requiring hours of data input. These requirements can interfere with patient interactions or result in clinicians spending additional time after work to meet clinical documentation requirements, both of which contribute to burnout.
Leading vendors in health IT
Following is a brief list of prominent vendors in healthcare IT:
- Athenahealth. Cloud-based services for EHRs, revenue cycle management and patient engagement.
- Epic Systems. Large-scale EHR software used by academic medical centers, community hospitals and healthcare systems.
- Greenway Health. EHR and practice management software optimized for small- to medium-sized practices.
- Meditech. EHR systems for hospitals and other healthcare organizations.
- Oracle Health (formerly Cerner Corporation). Healthcare IT systems, including EHRs, population health management and analytics.
- Veradigm (formerly Allscripts). EHRs, practice management and interoperability solutions.
How will AI affect the future of health IT?
AI is increasingly present in healthcare IT systems, thanks to its numerous benefits and use cases:
- Improved diagnostics. AI can rapidly analyze a vast amount of data -- such as images, X-rays, lab results and patient data -- to help diagnose conditions with incredible speed and precision.
- Personalized medicine. AI can help physicians more easily tailor treatments to a patient's unique needs by quickly analyzing genetic data, patient history and other metrics.
- Task automation. Routine tasks, such as scheduling, billing and documentation, can be automated using AI.
- Predictive analytics. By analyzing patient data and comparing it against larger data sets, AI can identify patterns that might indicate potential health issues; this can support preventive care.
- Real-time interactive healthcare. Telemedicine, chatbots and virtual medical assistants can all be enhanced using AI for language translation and symptom analysis.
- Medication development. AI can increase the speed and efficiency of drug development by analyzing large data sets in relation to existing and potential chemical compounds.
- Patient engagement. AI can help clinicians quickly respond to common patient queries, provide automated reminders and guidance, improve communications and encourage patients to follow treatment plans.
- Cybersecurity. AI can strengthen cybersecurity through rapid detection and mitigation of cyberthreats, helping to better protect patient data and healthcare IT and networks.
Health IT is critical to the present and future of healthcare, and AI is expected to play a growing role.
AI is transforming healthcare with predictive analytics, personalized treatments, and smarter care delivery. Explore the leading AI tools in healthcare today and the top ways AI is reshaping the industry.






