Salesforce Health Cloud roadmap boasts payer tools, CX, AI
Salesforce users in healthcare get tools that bring membership and benefits data and insurance utilization and claims data analysis tools into Health Cloud.
SAN FRANCISCO -- Salesforce Health Cloud's close relative, Health Cloud for Payers, has been pumped up with new tools for healthcare providers and payers to integrate patient insurance data and improve health plan member experience.
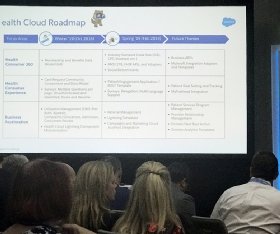
Salesforce laid out a path for the near and long-term future for both Health Clouds that include AI enhancements and chatbots, links to other Salesforce Cloud systems with its new Customer 360 product and the ability to incorporate social determinants of health.
Salesforce Health Cloud for Payers will see general release in October 2018 and February 2019 of new capabilities for complex care management, health plan membership, benefits and claims, insurance utilization management, quality measurement and member and provider services, the vendor said during its Dreamforce 18 conference here on Sept. 25.
Health Cloud value propositions
The CRM giant, which is this city's biggest tech employer and jams up downtown during its sprawling annual conference, first previewed Salesforce Health Cloud for Payers in early summer 2018.
Josh Newman, M.D., chief medical officer and director of product management and health strategy, said in an interview here that MuleSoft, the software integration vendor Salesforce bought earlier this year, worked on building the two health systems upon the Service Cloud framework.
"There are three big value propositions" with Salesforce Health Cloud, Newman said. "The first is member services; if you're happy and loyal, you become a good customer. The second is actually making people healthier. The third is building this network of all these physicians."
One of the key functions of Health Cloud for Payers that Salesforce touts is its ability to make care coordination easier for providers and payers.
Coordinating the efforts of physicians and other clinicians with payers has been a major part of the move to value-based care, in which providers are paid for better healthcare outcomes, not the number of procedures they do.
Salesforce Health Cloud and the payer version will help providers, payer-providers (provider-owned insurance plans), health plans, and employer-owned payer organizations better coordinate preventive care and help people with chronic conditions out of the hospital, Newman said.

Health Cloud users tout benefits
Meanwhile, at a packed Dreamforce panel session, a trio of corporate Health Cloud users talked about how the healthcare CRM system helps them manage healthcare costs, improve care quality and boost member satisfaction.
Martha Wofford, group vice president of commercial operations and patient experience and education at Davita, a national kidney care provider, said Health Cloud supports the clinical workflow of nurses who manage care for chronically ill patients, on behalf of payers.
"What Health Cloud really lets us do is be really dynamic in how we support patients, understand their needs and help our care team ... design interventions," Wofford said during the panel discussion. "It's just a completely flexible platform. You can do with it whatever you want."
While Davita has had good results with Salesforce Health Cloud, Wofford said in an interview after the session that perhaps because the provider started using the system not long after it was introduced in 2015, configuring it was a challenge.
Salesforce's vertical strategy
Salesforce Health Cloud and Health Cloud for Payers follow Salesforce founder and CEO Marc Benioff's strategy of exploring verticals that other CRM vendors might not, at the right time in those industries' evolution, said Matt Fleckenstein, a former Salesforce IoT Cloud vice president.
The development path to Health Cloud for Payers from the original Health Cloud was a typical Salesforce play, said Fleckenstein, currently Chief Product Officer at Nintex.
"Salesforce is very good at understanding a pattern and where they fit into it. Like starting with things like patient care," he said. "But when you get into things like claims management, the payer side of things, it's a bit more complex. They started in a place of their strengths, and as Salesforce often does, landed and then grew."
Pulling together disparate health data
Asked about the array of new tools and capabilities that Salesforce Health Cloud's designers have promised in their product development roadmap, Wofford, of Davita, said "we're excited to see some of the new things that become available."
William Symans, president and co-founder of Salesforce partner Saxa Solutions, a health IT and life sciences consulting firm, said after the panel he thinks Salesforce Health Cloud fills a void in patient experience and engagement and connecting, up to now, unconnected sources of data in healthcare.
"It's really interesting. They're closing a lot of the gaps and really solving some problems in the healthcare space that just aren't addressed today," Symans said.