Predictive analytics in healthcare: 12 valuable use cases
Predictive analytics' increasingly invasive presence in a host of healthcare applications yields more personalized patient care, earlier interventions and reduced hospital costs.
Predictive analytics in healthcare provides benefits mainly in clinical care, administrative tasks and operational management. More importantly, the technology is already delivering value in a multitude of healthcare settings, including small private physician practices, healthcare insurance companies and the largest academic hospitals.
Moreover, the use of predictive analytics in the healthcare industry is expected to become more prevalent. Electronic health records (EHR) systems already offer many predictive analytics capabilities, and analysts expect vendors to add even more capabilities in the future. Additionally, health IT providers are building their own analytics engines to help healthcare providers deliver optimal care. And they're partnering with healthcare institutions to build proprietary algorithms designed to improve clinical care, administrative performance and operational efficiency.
There are, of course, challenges to advancing the use of predictive analytics in healthcare. Healthcare institutions have limited dollars to invest, so they're cautious about deploying the technology until they're certain they'll see returns. Some of these facilities also must mature their data management programs to ensure they have the data necessary to make good use of any analytics capabilities. And vendors and healthcare entities must improve their collection, governance and sharing of high-quality data to advance the use of analytics technology.
Use cases for predictive analytics in healthcare
Despite these challenges -- which aren't unique to the medical industry -- the healthcare sector has been advancing its use of predictive analytics in recent years. Following are 12 of the more common applications of predictive analytics in healthcare.
1. Clinical predictions
Clinicians, healthcare organizations and health insurance companies use predictive analytics to articulate the likelihood of their patients developing certain medical conditions, such as cardiac problems, diabetes, stroke or COPD. "There's a lot of national data, EHR data, biometric data, claims data, and by pulling all that together, you can create models that can then be used on a national or community or even an individual level to predict the likelihood of these disease states," explained Nicole Bengtson, managing director at consultancy Huron and executive lead for its care transformation team. Health insurance companies were early adopters of this technology, and healthcare providers now use it to identify which patients need interventions to avert diseases and improve health outcomes.
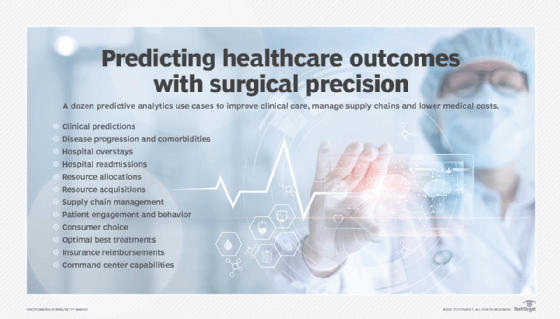
2. Disease progression and comorbidities
Similarly, healthcare institutions are using predictive analytics to identify patients whose conditions might worsen, said Adam Wilcox, director of the Center for Applied Clinical Informatics at Washington University School of Medicine and a member of the American Medical Informatics Association. They can use it, for example, to predict which diabetes patients are most likely to develop renal disease. Clinicians also use predictive analytics to identify patients whose conditions are progressing into sepsis. It's a critically important capability that can save lives, Wilcox said, because the ability to identify such disease progression in its early stages allows for the early interventions that can drastically improve outcomes for these patients. As is the case with many applications of predictive analytics in healthcare, however, the ability to use this technology to forecast how a patient's condition might progress is limited to certain conditions and far from universally deployed.
3. Hospital overstays
Healthcare organizations also use predictive analytics to identify which hospital inpatients are likely to exceed the average length of stay for their conditions by analyzing patient, clinical and departmental data. This insight allows clinicians to adjust care protocols to keep the patients' treatments and recoveries on track, said Peter Otto, an associate professor and director of healthcare analytics at Clarkson University. That in turn helps patients avoid overstays, which not only drive up costs and divert limited hospital resources, but also may endanger patients by keeping them in environments that could expose them to secondary infections.
4. Hospital readmissions
Another well-established and prevalent use of predictive analytics in healthcare is identifying patients at high risk of hospital readmission. Forecasting which patients may be readmitted after a hospital stay allows clinicians to adjust their post-hospitalization treatment plans, Bengtson explained, noting that reducing readmissions saves money, preserves healthcare resources for new patients and improves patient outcomes.
5. Resource allocations
The size, scope and complexity of healthcare organizations have made efficient and effective resource allocation difficult for administrators. But predictive analytics can identify patterns in resource allocations and predict future needs, thereby enabling administrators to acquire or move the right resources to the right place at the right time. "Patient utilization patterns, the overall capability of the organization, resources -- those used to be separate areas that are now coming together in a really fruitful way to help organizations manage their [operations]," Bengtson said. Predictive analytics "helps organizations to manage their operations much better."
6. Resource acquisitions
Similarly, healthcare organizations use predictive analytics to identify what additional resources would most likely be needed based on data points like seasonal needs, expected demographic changes and patient populations. Otto said a hospital can use analytics to predict whether it needs to invest in one or more CT scanners based on future anticipated needs; the analytics engine can also predict what additional resources will be needed to operate those scanners for the anticipated case load. "Then [the healthcare institution] can plan and staff resources appropriately," Otto noted, rather than invest in costly equipment and expertise that may be underutilized or be left without needed resources when it's required.
7. Supply chain management
Healthcare entities are using predictive tools to better manage their supply chains, just as companies in most other industries. Healthcare organizations, Bengtson reasoned, can gain visibility into their vast and complex supply requirements and predict which streamlined purchases and vendor consolidations could save money, reduce waste and provide efficiencies.
8. Patient engagement and behavior
Predictive analytics allows healthcare entities to better understand and engage their patients individually and as part of larger demographic groups, said Kumar Chebrolu, managing director and healthcare AI practice leader at Deloitte. Predictive analytics, for example, can help determine which patients are likely to be no-shows for their appointments -- information that can help administrators better plan clinician schedules and allocate resources. The advanced technology can be used to predict which patients are most likely to adhere to a prescribed medication regimen and which ones won't. It can also predict which interventions or healthcare messages would resonate best with certain patients or patient populations. All this information allows advocates to more effectively work with patients to improve their healthcare outcomes.
9. Consumer choice
Predictive analytics is also beginning to be used to help people pick their providers, Bengtson said, explaining that the analytics engines can analyze clinician data to predict which clinician best fits the patient's needs. This capability goes beyond generating for patients a list of doctors in the area or with the medical specialty they need. Rather, the technology predicts the specialists that best match a patient's specific requirements, such as offering a list of providers with evening and weekend hours and immediate availability.
10. Optimal best treatments
Treatments for certain conditions, such as some cancers, should be tailored to the patients and their diseases to achieve the best patient outcomes. But no individual can analyze all the data required to make those treatment decisions, which is where predictive analytics technology comes in. Although still emerging, this technology is expected to be capable of analyzing, for example, the genomics of a specific cancer and the patient diagnosed with the disease to predict the optimal treatment regimen, said Gartner senior director analyst Seth Feder. That capability is particularly critical for treating quickly progressing diseases when physicians don't have time to try different approaches before deciding on the best option.
11. Insurance reimbursements
Billing is another administrative area that gets a boost from predictive analytics, Feder said. Healthcare entities can analyze the documentation they're submitting to insurers to identify claims that are likely to be declined and those that could yield higher payments. "It's used to optimize financial performance," Feder said, explaining that the technology looks for missing or insufficient reimbursement codes and identifies "opportunity to upcode."
12. Centralized command center capabilities
Health IT vendors are now pulling together many of these predictive analytics use cases to give healthcare institutions the ability to manage them all together, in what analysts at Gartner are calling real-time health system command center capabilities. "It's like an air traffic control system that tracks the environment," Feder said. "It creates a pervasive situational awareness solution for a health system that will drive decision-making." It could predict everything from the likely number of available ICU beds to supply needs to in-patient bed availability, he added. This system, for example, can alert administrators to likely shortfalls in bed availability or in the number of nurses based on anticipated demand for services. Administrators can then act in advance to create better patient experiences and ultimately better outcomes. "That's maybe two to five years away from mainstream adoption," Feder conjectured, "but we think it's going to be transformational."
Benefits of predictive analytics in healthcare
Predictive analytics provides several key benefits, including more personalized, effective and consistent patient care, earlier medical interventions, streamlined hospital administration and reductions in healthcare costs.
1. Improved patient outcomes
Predictive analytics is being used to identify optimal treatment plans, medication regimens and engagement material, as well as predict disease progression and likely comorbidities in a limited number of cases today. But those applications alone are significantly improving patient care and outcomes by allowing for earlier and more effective medical interventions.
2. More consistent care among patients
The availability of experienced, highly trained administrators and clinicians varies, meaning some patients may have access to higher quality of care than others. The use of predictive analytics can help ensure that expert insights are equally distributed among patients. An experienced critical care nurse, for example, may be better able to identify patients likely to develop sepsis than a well-trained but less experienced nurse. The junior nurse, however, can use predictive analytics to boost the level of care for patients equal to that of the more senior caregiver.
3. Operations efficiency and cost savings
Predictive analytics enables earlier and more effective medical interventions, as well as more efficient healthcare administration and operations management, resulting in cost reductions. Clarkson's Otto noted that a daylong hospital stay costs about $3,500. Hospitals that use predictive analytics to reduce or eliminate unnecessary overstays, he said, can help control the country's spiraling healthcare costs and redirect costly, limited health resources away from patients no longer in need to those in greater need.







