
Getty Images
Key Strategies for Health Systems to Achieve Economies of Scale
Selecting the right scale model and motivating facilities to work together are methods for health systems to realize savings from economies of scale.
Companies from across industries use economies of scale to realize cost savings. While hospitals and health systems are borrowing the economic concept to reduce spending, many healthcare organizations have encountered challenges with achieving the benefits of economies of scale.
The Healthcare Financial Management Association (HFMA) defines economies of scale as the “gains provided through the consolidation of effort or volume.” In other words, companies can lower the per-unit fixed costs of their goods by generating a greater quantity of the good. Costs are spread over a larger number of products, therefore realizing savings for the company.
As claim reimbursement rates fall across public and private payers, hospitals and health systems are under increasing pressure to contain their costs. Achieving economies of scale is a key strategy for larger healthcare organizations to reduce and control their costs, according to about 29 percent of hospital executives who plan to use this strategy in 2017.
Large organizations are turning to healthcare mergers and acquisitions to implement economies of scale strategies. Healthcare merger and acquisition activities recently increased by 15 percent in the second quarter of 2017 compared to the previous quarter.
Kaufman, Hall & Associates’ Managing Director Patrick Allen attributed the rise in healthcare mergers to health systems “thinking strategically about how best to build the scale and capabilities needed to remain competitive in a rapidly changing healthcare environment.”
Realizing the gains through economies of scale is possible, with potential savings between 15 and 30 percent, a 2016 Strategy& report stated. But many healthcare organizations do not see these gains and are instead left with the high costs of taking on another care site.
Their analysis of over 500 health systems and over 5,600 individual facilities revealed that health systems comprising several facilities do not experience lower costs resulting from scaling methods.
Although stand-alone hospitals are more likely to produce economies of scale, the research showed.
What causes health systems to never realize cost savings from implementing economies of scale? How can healthcare organizations overcome these challenges?
Select the appropriate economies of scale model
Healthcare organizations usually turn to a merger or acquisition to launch an economies of scale project. But the typical healthcare merger approach may not be appropriate for every organization, McKinsey & Company researchers stated.
Researchers developed what they called the “smarter scale equation,” which responds to recent regulatory challenges of healthcare mergers. The Federal Trade Commission (FTC) recently increased their scrutiny of hospital and system deals by attempting to block several announced deals.
“Vigorous enforcement of the antitrust laws is more important than ever,” FTC Chair Edith Ramirez said, speaking to attendees of the 2016 American Health Lawyers Association’s Antitrust in Healthcare Conference. “We will continue to use all of the tools at our disposal to promote the robust competition that underpins healthcare reform, benefiting consumers through lower costs, better outcomes and greater access to care and innovation.”
In light of increased merger blocks from the FTC, researchers advised health systems to consider the traditional model alongside alternative scale models, including:
• Classic economies of scale: emphasizes lowering base per unit costs by spreading the fixed costs across a greater volume of patients and/or by allowing providers to negotiate lower prices for major services
• Economies of scope: allows providers to leverage their scale to create non-traditional revenue streams, such as direct-to-employer offerings
• Economies of structure: enables providers to gain access to capital at lower costs and stronger negotiation power with payers, may also allow providers to take advantage of a broader footprint across the care spectrum and assume risk pooling for population health management
• Economies of skill: permits providers to increase their capabilities and improve their performance through sharing or building of best practices at comparatively lower costs
Once a health system decides on the scale model, the organization can use four methods for implementation. First, health systems can engage in inorganic scale, which encompasses healthcare merger and acquisition activities.
Second, health systems can opt for virtual hospital integration. This method allows systems to leverage scale benefits without directly controlling another organization or committing to a long-term collaboration. Examples include co-provision, outsourcing of shared services, and joint development of knowledge and innovation.
Third, horizontal organic scale involves a health system stretching its footprint across the care spectrum. A health system may choose to get involved with physician practices or outpatient facilities to grow the hospital setting.
Finally, health systems can use the vertical organic scale method to directly develop relationships with payers, employers, or both to increase patient volume. This approach is typically coupled with horizontal expansion, especially when providers and payers aim to create new care or payment models.
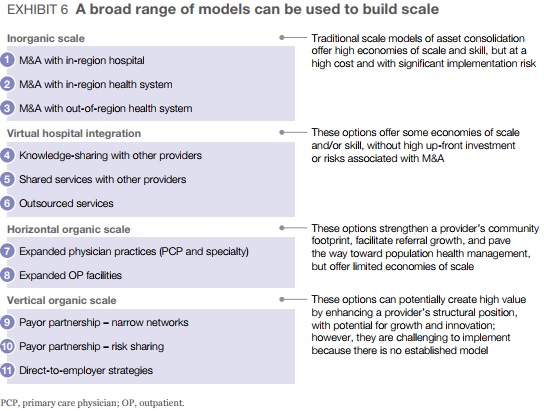
Health systems should assess the potential risk and benefits of each scale model and implementation method, researchers recommended.
Encourage facilities to work as one rather than independently
While not all economies of scale strategies involve a complete merger, achieving scale does include working with independent facilities under one mission. But motivating facilities within a health system to give up their autonomy is a major hurdle that health systems face when achieving economies of scale.
Healthcare is a personalized industry. Providers aim to deliver individualized, patient-centered care to all of their patients. They must also respond to local community health needs.
Care site leaders often believe they can deliver the highest value, personalized care by managing core business and clinical functions independently of their system.
However, realizing cost savings under economies of scale models relies on facilities working as one.
Strategy& advisors recommended that health systems restructure their operating model to emphasize accountability and control at the system level.
“The objective is to strike the right balance of centralized control over most transactional operations, such as reporting, while accommodating local nuances in areas where it truly matters, such as pre-procedure education,” they wrote.
The operating model should include the following three components:
• Corporate Core: manages corporate governance, policies, and services for corporate strategy, financial operations (eg, tax, treasury, accounting controls, reporting, and auditing), human resources, and health IT
• Shared services centers: act as central sources for expertise and scale, providing resources for management of financial operations, revenue cycle, supply chain, human resources, health IT, service lines, clinical services, and nursing
• Operating units in regions and facilities: handle patient care procedures and other factors that affect financial performance, including ancillary services, physician contracts, revenue cycle management
Health systems should also restructure roles and decision rights to implement the operating model. For example, corporate core entities should define organizational goals, rationalize the portfolio, set performance targets, and approve investments and budgets, whereas facility leadership should only be responsible for operating and tracking performance.
The redesigned governance structure should include incentives at the system and facility level to encourage collaboration and advanced overall performance, the advisors added.
Standardize clinical process across facilities
As part of the challenge of encouraging independent facilities to operate as a single system, health systems frequently encounter a patchwork of clinical processes. System leaders must standardize processes to drive economies of scale across the system.
Clinical standardization can help health systems realize the benefits of scale by lowering costs and enabling providers to follow the same protocol for high-value care. Care variations resulted in cost differences of 8.4 percent among hospitalists within the same facility and 7 percent among hospitalists across facilities.
The process of standardizing clinical processes can reduce the cost variations experienced within and across hospitals, explained Bart Hill, MD, St. Luke’s Health System’s Vice President and Chief Quality Officer.
“When you standardize your processes and you perform consistently, we have seen fewer of those occurrences that ultimately add extra cost without value, such as readmissions, longer lengths of stay, and more complications,” he recently told RevCycleIntelligence.com.
Health systems should turn to their physicians rather than take a top-down approach to implement standardized care protocols, Strategy& advisors stated. Systems should create multi-functional, physician-led teams to define clinical goals and develop processes early during a healthcare merger or collaboration commitment.
The team could also help health systems to prioritize medical and surgical specialties to rationalize and create a plan to achieve merger synergies.
The collaborative nature of the physician-led team should also boost buy-in at all levels, improve morale, and increase the chances that new clinical processes will continue.
Remove redundant service lines
Once a health system acquires or partners with another organization to achieve economies of scale, leaders may find that facilities in close proximity contain many of the same service lines.
Health systems should eliminate redundant service lines to reduce costs and improve efficiency, Strategy& advisors suggested.
Leaders should examine the supply and demand of certain services in terms of market and disease-related activities as well as explore market competition and patient preferences. They should also assess how profitable service lines are across different sites of care.
For example, an academic medical center that has merged with two community medical centers in the same market may offer overlapping cancer care services. By assessing services lines, the health system could find that costs would decrease if the community medical centers managed primary and secondary services, while the academic medical center handled more complex procedures and services.
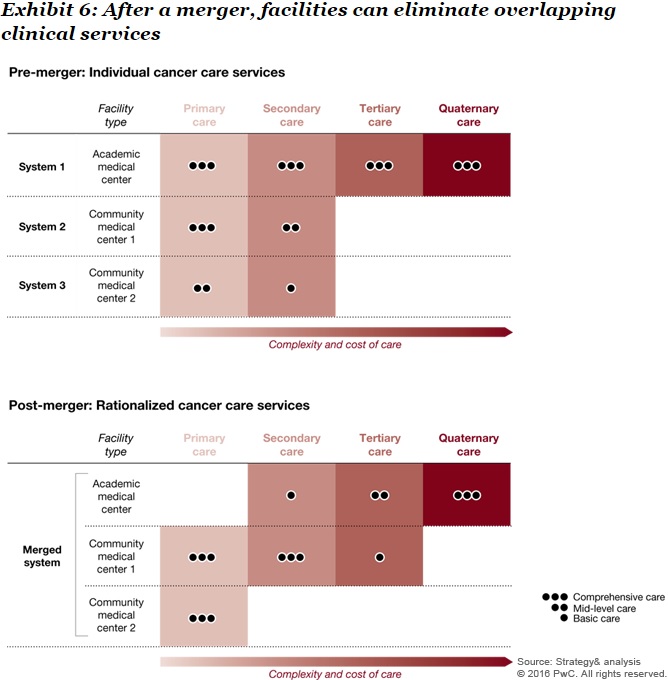
Similarly, health systems may determine that one hospital in its system should not deliver specific services because they are not profitable to furnish in that setting.
Mercy experienced this situation when the system entered into a management contract with a critical access hospital in Oklahoma, HFMA reported. The system recommended that the hospital eliminate its obstetrics department because the hospital only had 70 deliveries in the past year. The service volume did not justify the costs associated with running a full department at that specific care site.
Health system leaders also questioned the care quality of the services since the number of deliveries was so low.
Despite several challenges of achieving economies of scale, researchers stated that realizing 15 percent to 30 percent in cost savings is possible for health systems. But each facility must work as one under the health system to achieve cost reductions.







