
Getty Images/iStockphoto
Providers Say Cost Transparency Will Improve Value-Based Care
Collaboration for value-based contracting would be improved with increased cost transparency, providers reported in a recent Insights by Xtelligent Healthcare Media survey.
As the healthcare industry continues to move towards value-based reimbursement, providers are calling for increased cost transparency to succeed in these models.
Earlier work from Insights by Xtelligent Healthcare Media showed that while many organizations were participating in value-based care models, these models were similar to fee-for-service. Value-based payments such as pay-for-performance or bundled payment models are relatively low risk for providers to enter.
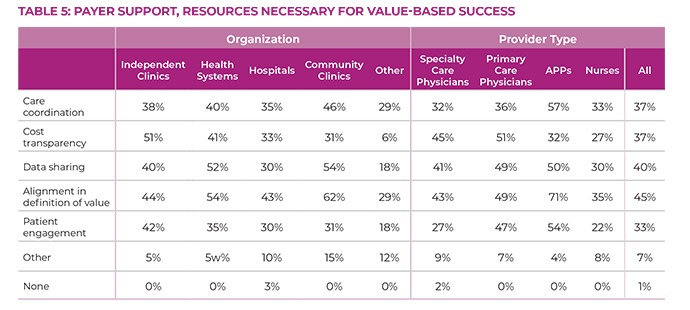
Riskier models such as downside risk or capitation, however, ask providers to take on larger financial risk for their patients. Insight's most recent survey revealed that, in order to succeed in riskier models, providers need different resources based on what type of medicine they practice and where they practice it.
The survey aimed to understand provider perceptions of value-based care. Specialty care physicians, primary care physicians, advanced practice providers (APPs) such as physician assistants and nurse practitioners, and nurses gave their opinions about partnering with payers for value-based reimbursement.
Results highlighted the resources providers need to succeed in these models and their confidence in their payer partnerships.
Critical to success was price transparency. Overall, 37 percent of respondents said cost transparency was a key resource they needed from payers. But physicians and providers in independent clinics were more likely to want this resource than other providers practicing in larger organizations.
Only 27 percent of nurses and 32 percent of APPs said they wanted these resources from payers. Even fewer said cost transparency would improve collaboration between payers and providers, with 4 percent and 21 percent of nurses and APPS reporting such, respectively.
These providers are more likely than their physician counterparts to be salaried, so their reimbursement is not linked to improving value.
Physicians, on the other hand, are likely to have their payment linked directly to their ability to reduce costs while improving quality. So they need a better understanding of the costs of care.
As a result, 51 percent of primary care physicians and 45 percent of specialty care physicians said cost transparency from payers would help them succeed in value-based care models.
Survey results also highlighted a breakdown by organizational size. Larger organizations have bigger bargaining power, with their own research to support value-based contracting and understand costs. They also often have greater financial resources, so assuming downside risk is less financially risky.
Only 33 percent of hospitals and 41 percent of health systems reported wanting cost transparency from payers while 51 percent of independent clinics reported the same. These independent clinics have a smaller market share and less bargaining power when negotiating value-based contracts, so they need cost information from payers in order to feel more confident when entering into agreements.
After the survey was complete, respondents were asked if they were willing to complete qualitative follow-up about survey results. Four interviewees provided context for the survey findings, highlighting real-world challenges related to working with payers on value-based care models and articulating key strategies.
Their responses underscore the fact that provider confidence to negotiate value-based agreements varies drastically based on the resources available to them.
In order to succeed in value-based care models, providers and payers need to level the playing field and align their goals. This cannot happen without more cost transparency, which allows providers to feel more confident in lowering care costs while improving care quality.
Only when payers and providers are on the same page and understand what the other needs will the industry truly be able to transition fully to value-based care.
Provider Perceptions of Value-Based Care also highlights provider motivation for participating in value-based care models, provider satisfaction with their private and public payer relationships, organization concerns with cost transparency, and challenges to collaborating with payers. The full report can be found here.







