
Getty Images
Preparing Providers for Full MACRA Implementation in 2022
ACOs and hospital-based providers will be most impacted by upcoming changes to quality scoring under full MACRA implementation, but with some work, they also have a lot to gain.
With the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), CMS did away with the Sustainable Growth Rate model. Now, they are able to reward high-value, high-quality Medicare clinicians with payment increases, while at the same time reducing payments to those clinicians who aren't meeting performance standards.
CMS intentionally wanted to make sure that the MACRA program was going to get full participation by all or almost all physicians in the country. They wanted to have not only robust participation, but also good performance across the program. So, they created a ramp-up period between 2017 and 2022, with lower performance thresholds that would make it easier for hospital-based providers to achieve higher scores.
The program has indeed had very high participation, with almost every provider in the country participating in MACRA from the first year. And performance has been good as well.
But a big part of MACRA reimbursement comes from a pool that Congress defined as revenue-neutral, or otherwise known as a penalty pool. With such high participation and performance, though, almost no one contributed to that pool.
In 2018, only about 3 percent of the providers in the country paid penalties. Therefore, there was no penalty pool to distribute. 2019 was even worse because people who exhibited poor performance were able to claim a COVID exemption – and our data shows that only 1 percent of providers actually paid a penalty.
Moving forward, those numbers are going to get much bigger. The bottom line is that there's a lot more risk, and theoretically, half of providers in the country will be penalized in order for funds to be available for the high performers.
Full MACRA rollout will push down performance scores in 2022
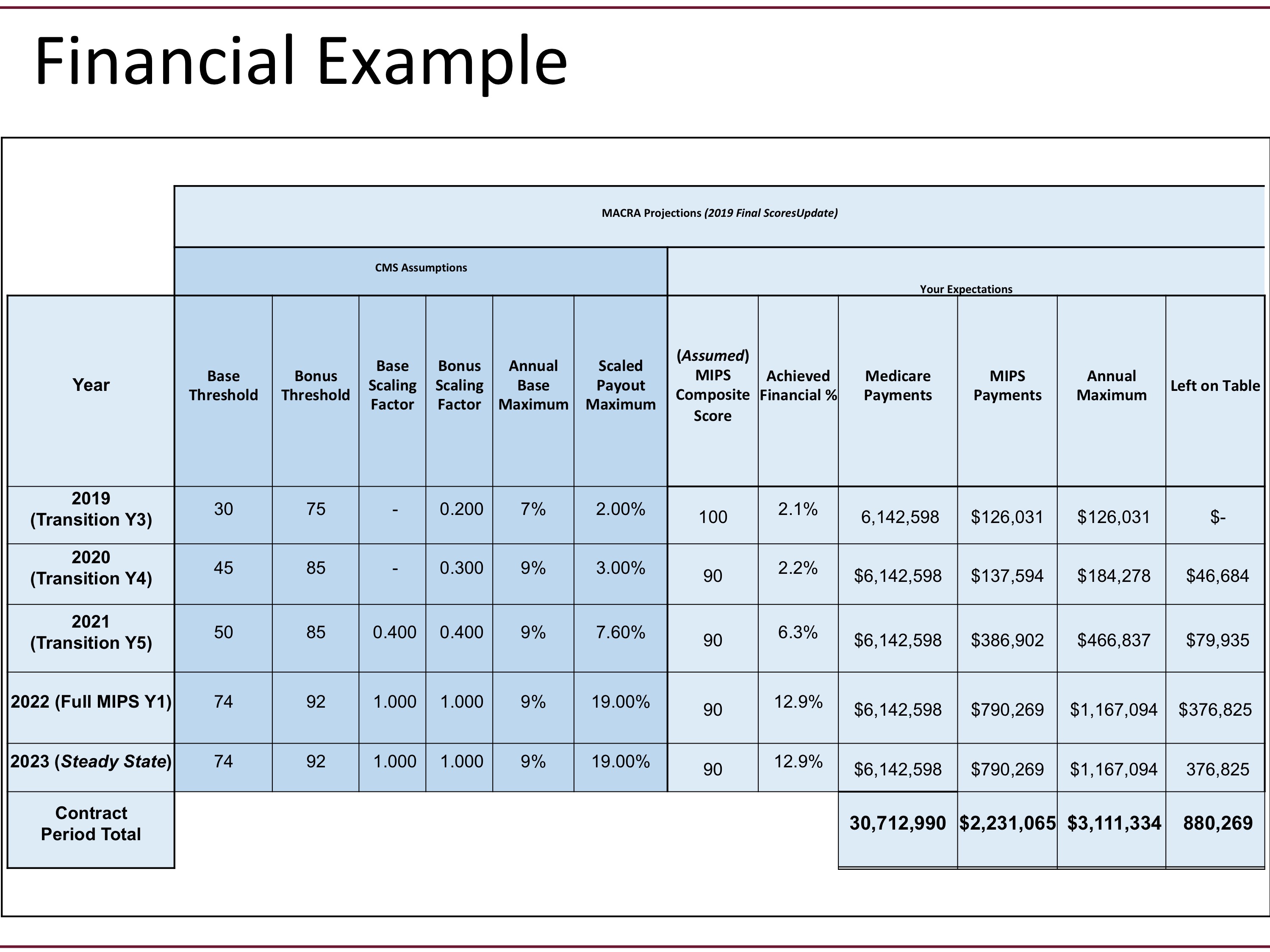
As the transitional period nears its end, the performance threshold is getting higher and it starts to approach the performance that people have actually been achieving. However, as evident in the graphic above, CMS is projecting a mean or median performance threshold of around 74 points – which means they’re projecting scores to go down.
But why? The first thing to understand is that, once the full MACRA program rolls out, performance on the Quality category will make up between 50 and 85 percent of a clinician’s overall score (especially for hospital-based providers).
There are also three major changes that will impact the MACRA program in short term:
- Starting in 2022, Quality scoring will also shift to the decile ranking system – so that if a clinician ends up in a lower percentile based on performance score, the clinician will only receive a single point or possibly a fraction of a point. Essentially, all safety nets go away under the scoring system.
- The ability to report Quality on only a portion of measures gets much more rigorous starting in 2022, otherwise known as the “case minimum” or the “data completion percentage.”
- Benchmarking also gets much more rigorous in 2022. Quality measures are based on a numerator and a denominator. The numerator is what percentage of the time providers are compliant with a given protocol or quality practice, and the denominator takes into account the patients that contributed to that. The result is a clinician’s performance rate on that Quality measure. So, for example, a performance score of 90 percent might sound good, but it may not benefit a clinician’s individual performance score if everybody else is scoring 92 or better. In that scenario, a clinician may only get one or two points. And since the minimum score goes away, clinicians could receive no points at all.
Additionally, there’s the plan for CMS to retire a batch of measures every year. The agency will most likely target the “easy” measures that many clinicians have submitted in the past.
These changes are going to be the big drivers pushing scores down to what CMS is projecting in the mid-70s for 2022.
Calculating the penalty/bonus performance threshold
Another big change that’s coming in 2022 has to do with the performance threshold that CMS uses to determine who gets penalized or rewarded. In the past, CMS has set the performance threshold at a gradually increasing rate. But, starting in 2022, that number is determined by the composite score of all providers in that given year.
There’s a big emphasis on how that number is calculated. And, by early next year, CMS must decide whether to use the “mean” or the “median” composite score (for all providers) in their calculation. The caveat, though, is that the composite score won’t be released until the middle of the following year. So, there will be about six months where clinicians will know their scores, but they won’t actually know whether that’s a good score or not.
The only way to protect reimbursement is to aim for extremely high scores. And, it’s a worthwhile effort because reimbursement increases will be dramatic for the top quarter-percentile that qualifies for a performance bonus.
Who will be impacted the most by MACRA changes?
ACOs will be one of the main groups impacted by upcoming changes to the MACRA program. Starting in 2021, they will no longer be managing the Quality reporting for their physician groups. Therefore, ambulatory providers will need to start analyzing and submitting their measures from their EHR.
But other providers, such as hospital-based providers, generally don’t have the EHR necessary to generate MIPS measures, which means that these groups will need to contract with a certified registry or QCDR.
How ambulatory providers can prepare
To help protect reimbursement, eligible clinicians should use the “Monthly MACRA Blueprint” concept, which places a heavy focus on ongoing reporting and active management throughout the year.
Many registries/QCDRs offer passive reporting options, but strategic groups should be looking at the broader picture and studying areas such as regulatory impacts, remittance reconciliation, targeted reviews, proper measure selection, and shortfall analysis to make sure performance is staying on pace.
Improvement Activities should also be built into regular practice. Pick these in advance and add documentation guidelines to provider resources to optimize performance under this MACRA category.
Finally, it’s also imperative that clinicians focus on clinical quality measure (CQM) improvement. Analyze data at the individual-physician level, even if the plan is to submit as a group, and look at high and low performers for insight.
_____________________________________________________________
Article Contributers:
- Dr. Andrea Brault – President & CEO, Brault Practice Solutions
- Jay Fisher – Partner, C3 Partners, LLC.
- Leann Lawson – Exec. Dir. of integrity, Education and MIPS – Brault Practice Solutions
About Brault:
Brault is a revenue cycle and practice management organization that partners exclusively with hospitals and acute care physician groups. Their intelligent practice solutions include MIPS optimization, practice analytics, and provider documentation training. Learn more at www.Brault.us
About C3 Partners, LLC:
C3 Partners provides next-level MACRA Optimization through unique tools and powerful collaboration, as outlined in a clear Monthly MACRA blueprint. See www.MACRAmonitor.com for more details.


