
Getty Images
2024 MIPS Changes and Their Impact on Emergency Medicine
CMS continues to shift the MIPS reporting process with a new model specifically designed to align with physician specialties, like emergency medicine.
The Merit-Based Incentive Payment System (MIPS) is a mandatory quality payment system for clinicians who receive Medicare Part B payments unless they qualify for an exception or are part of an alternative payment model (APM). More than 655,000 eligible clinicians engaged with the MIPS program in 2021, according to the latest data from CMS.
The program is meant to allow clinicians to earn incentive payments for providing high-quality care. However, MIPS has been scrutinized since its launch in 2017 for its reporting requirements, particularly those concerning specialty physicians and groups.
Many of the quality measures traditionally used to assess performance in MIPS were based around primary care, which is the most common point-of-service where Medicare beneficiaries received treatment. This has caused other specialty providers to force fit quality measures or risk a negative adjustment.
CMS has worked to address specialty physicians' challenges with MIPS reporting, most recently introducing a new reporting option for eligible clinicians: MIPS Value Pathways (MVPs).
From traditional MIPS to MVP reporting
MVPs provide specialty physicians with a more tailored approach to MIPS reporting. The 16 MVPs available in 2024 offer more aligned quality measures, but specialty physicians such as those in emergency medicine (EM) will need to study their MIPS reporting strategy to determine whether a shift to the MVP would benefit their overall MIPS score.
In the 2024 performance year, there are 16 MVPs eligible clinicians can use to report data to MIPS. The MVPs range from specialty-specific, with tracks tailored to EM and primary care, for example, as well as condition-specific, such as the neurodegenerative conditions or kidney health MVPs.
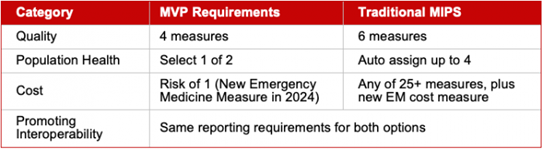
Quality reporting requirements differ from traditional MIPS. For example, the “Adopting Best Practices and Promoting Patient Safety within Emergency Medicine” MVP requires eligible clinicians to report four quality measures, including at least one outcome measure. In traditional MIPS, eligible clinicians must report six quality measures.
EM clinicians can also select up to two population health measures rather than risk having up to four attributed to them.
Finally, there is just one cost measure in the EM-specific MVP, whereas the traditional MIPS track contains 29 cost measures, which count towards 30 percent of a clinician’s final MIPS score.
CMS believes this approach to MIPS reporting moves away from siloed activities and quality measures toward more clinically related, relevant, and meaningful activities and measures. MVPs are meant to be the future of MIPS reporting, with CMS transitioning traditional MIPS to this more tailored approach.
Evolution of MIPS scoring
In traditional MIPS, four performance categories make up an eligible clinician’s final score: Quality (30 percent), Promoting Interoperability (25 percent), Improvement Activities (15 percent), and Cost (30 percent). However, because of misalignment with specialty care delivery, EM clinicians have not been subject to the traditional breakdown. Historically, the Cost and Promoting Interoperability categories have not applied to EM clinicians.
“Instead, the weight of those categories was shifted to Quality. So, the Quality category made up 85 percent of their total score, and for the past several years, the strategy for EM physicians was to optimize their Quality score,” says Dr. Andrea Brault, MMM, FACEP, president and CEO of Brault. “But, in recent years, the strategy has shifted as CMS continues moving toward the MVP model and adding more emphasis on Cost and Population Health.”

EM clinicians electing to report through the MVP will need to consider a broader performance strategy that includes quality optimization, population health work, and cost containment.
Population health, cost categories are wildcards
MVPs allow EM clinicians to report on more aligned, clinically relevant measures, which could translate to higher overall performance scores. However, clinicians should make an effort to understand the MIPS categories that are new to them, as these may present some challenges with MIPS reporting.
“Population health scores are calculated in the background by CMS and added to your Quality score at the end of each performance year,” Dr. Brault explains. “So, physicians are typically unaware of which measures they’ll receive attribution on, and they have no way of impacting those scores. So, they’re a bit of a wildcard and a big unknown. This is a relatively new concept for EM physicians, but in recent years, more physicians have started to be attributed one or two population health measures.”
In 2024, the four population health measures that may be attributed to EM clinicians are:
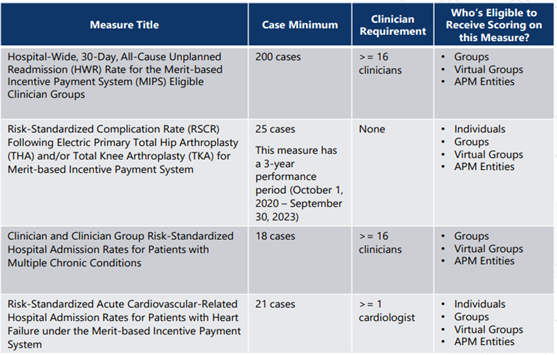
“This is where the strategy might shift for physicians already seeing score attributions in this area,” Dr. Brault states. “For those physicians, joining the MVP could be a way for them to limit their exposure to other population health measures since MVPs self-select only one population health measure and are not scored on the others. On the other hand, physicians who’ve never received a population health score may not want to add additional risk by joining the MVP.”
Similarly, one of the new 2024 Cost measures is specific to EM clinicians, and the score will be calculated in the background by CMS. Every EM physician will receive attribution for this Cost measure, whether in traditional MIPS or the MVP – and the percentiles will be adjusted so that there are winners and losers. But, there isn’t much they can do at this point except wait and see how this new cost measure will be scored and evaluated, explains Dr. Brault.
“There are still many unknowns for EM clinicians,” says Dr. Brault. “But these recent shifts to the MIPS grading criteria should be closely monitored, especially as more clinicians are penalized and as the penalties become more material. Physicians should also note that they can report through multiple tracks and CMS will award the highest of all scores. So, for those who are able, it might be worth doing both traditional MIPS and the MVP and seeing which one fares better.”
For those who want to register for the MVP option, the registration window is open April 1 – December 2. Learn more about MVP registration.
_________________________
ABOUT BRAULT PRACTICE SOLUTIONS
Brault is a revenue cycle and practice management organization that partners with hospitals and independent physician groups. Their intelligent practice solutions include coding and billing, MIPS optimization, provider documentation training, and practice management. Learn more at www.Brault.us




