
Getty Images
Observation Care CPT Updates to Impact Emergency Physician Reimbursement
New 2023 CPT guidelines for patients in observation status classify this care as an inpatient service and add new requirements for emergency physician reimbursement.
The American Medical Association (AMA) has released new CPT guidelines for patients in Observation status, including some that may significantly impact emergency physician reimbursement. These updates include new CPT codes, documentation rules, and coding requirements.
“Observation services are becoming more common in the emergency department, and they play an important role in mitigating unnecessary hospital admissions,” explains Dr. Andrea Brault, President and CEO of Brault Practice Solutions. “If we think of it like a traffic signal, green would be patients we are confident can be successfully treated in the ED. Red would be patients who require quick admission into the hospital. And Yellow would be the patients in Observation status who need more time to determine their medical trajectory.”
These services fall into the middle ground between the hospital and emergency department, and there are important rules to keep in mind from a reimbursement perspective
Observation services will now be billed under the Inpatient CPT codes.
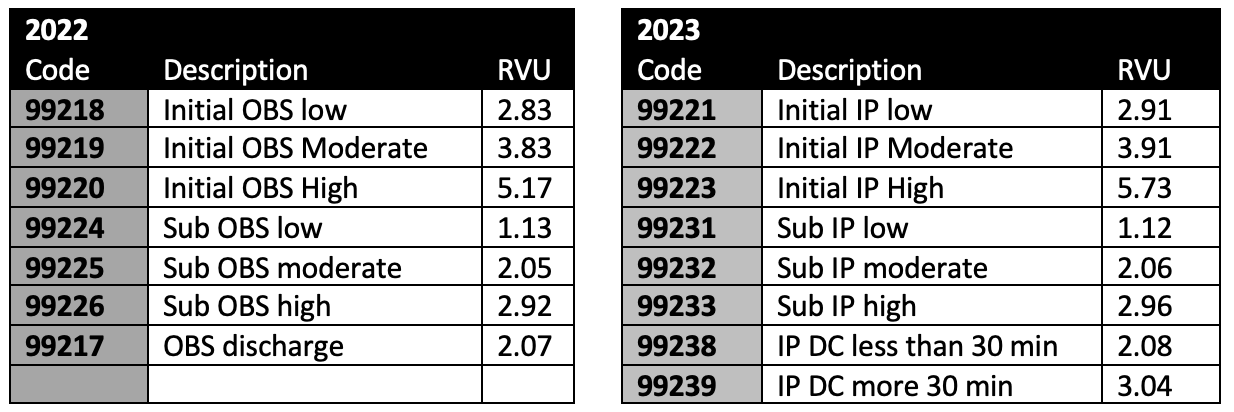
AMA and CMS have both agreed to eliminate the different day and subsequent day Observation codes in 2023. Instead, they will add observation services to the description of inpatient codes.
For patients designated/admitted as “observation status” in a hospital, it is not necessary that the patient be located in an observation area designated by the hospital. If such an area does exist in a hospital (as a separate unit in the hospital, in the emergency department, etc.), these codes may be utilized if the patient is placed in such an area.
“This language indicates that these inpatient codes can be used for observation status patients with beds in the emergency department,” explains Dr. Brault. "And it's generally believed that this shift to Inpatient codes will increase RVUs for observation services beginning in 2023."
Assuming no major changes, RVUs for 2023 observation status should increase compared to 2022.
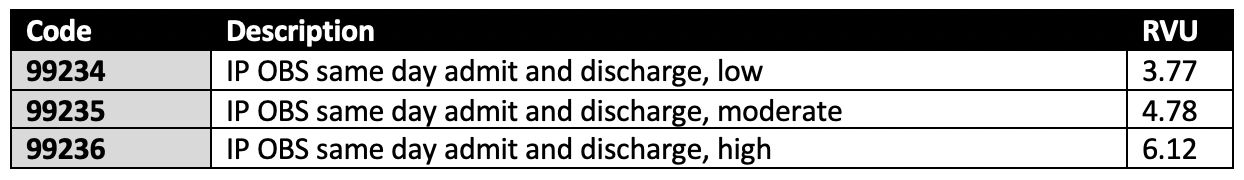
However, some observation CPT codes will not be changing. For example, the codes for admit discharge on the same date of service (DOS).
Emergency physicians need to document their time spent on Observation care
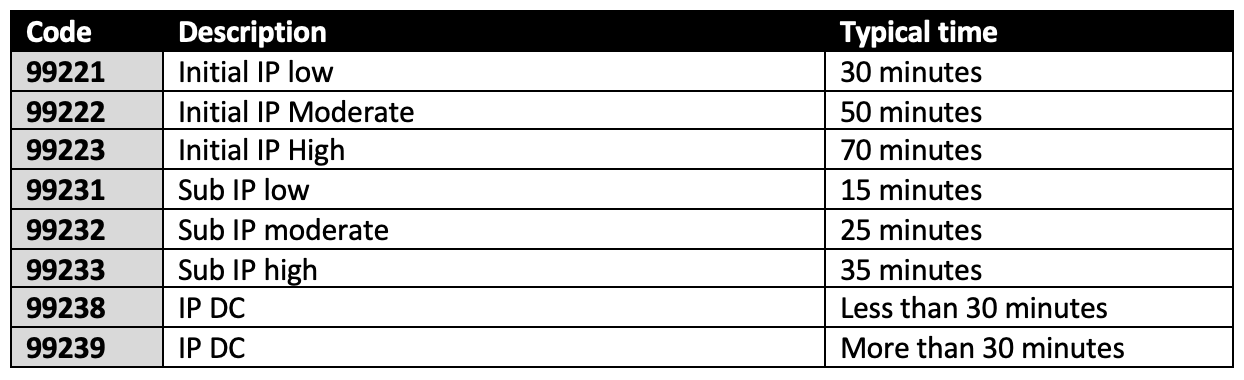
Moving observation services to the inpatient code sets will also shift the rules for determining a patient’s level of care. The most common CPT codes used in the emergency department are evaluation and management codes, where a level of care is determined solely on medical decision-making (MDM) criteria. But, as an inpatient code, observation care will now include a time element.
“The level of observation status can be based on either MDM or time,” explains Dr. Brault. “So, it’s important for physicians to document their total time spent on Observation care – as it could help justify a higher level of care.”
Physicians should document the total time spent on observation care on the date of the encounter. This can include face-to-face time, time spent with a family member or caregiver, and non-face-to-face time the physician spends on the patient. However, this calculation should not include time spent on separately billable activities such as interpreting an EKG.
Time requirements for each level of inpatient observation status:
But, guidelines may differ between commercial, government payers
Dr. Brault explains, “One key difference between the CPT and CMS guidelines is the ability to classify an observation encounter as a separately billable event, in addition to the emergency department evaluation and management services.”
AMA has stated that the same physician can bill visits from two different statuses on the same date of service (DOS) if each encounter is documented separately.
When the patient is admitted to the hospital as an inpatient or to observation status in the course of an encounter in another site of service (e.g., hospital emergency department, office, nursing facility), the services in the initial site may be separately reported. Modifier 25 may be added to the other evaluation and management service to indicate a significant, separately identifiable service by the same physician or other qualified health care professional was performed on the same date…
However, CMS has indicated in their 2023 Proposed Final Rule that they will not follow these guidelines and will only pay for one visit on the same DOS by the same physician.
We also propose to retain our current billing policy in the Medicare Claims Processing Manual, IOM 100-04, Chapter 12, 30.6.1.A. that a physician may bill only for an initial hospital or observation care service if the physician sees a patient in the ED and decides to either place the patient in observation status or admit the patient as a hospital inpatient…
“This is an important distinction that will impact a significant portion of claims, and we fear that commercial payers may now want to consider using the more restrictive CMS guidelines as a way to lower their overall physician payments,” explains Dr. Brault. “It’s too soon to tell what the broader impacts will be, but at the very least, we know that this will create new documentation requirements for emergency medicine providers and additional steps for their RCM teams to submit each claim properly."
_____________________________________
Article Contributor:
Dr. Andrea Brault, President and CEO at Brault Practice Solutions.
ABOUT BRAULT PRACTICE SOLUTIONS
Brault is a revenue cycle and practice management organization that partners with hospitals and independent physician groups. Their intelligent practice solutions include coding and billing, MIPS optimization, provider documentation training, and practice management. Learn more at www.Brault.us
For more information on the 2023 CPT guideline changes, visit https://www.ama-assn.org/system/files/2023-e-m-descriptors-guidelines.pdf



