
gmast3r/istock via Getty Images
Top Revenue Cycle Management Vendors and How to Select One
Epic Systems and MEDITECH topped the revenue cycle management vendor list, but the market is expected to change in the next year.
As value-based reimbursement models, such as the upcoming Quality Payment Program, break down the walls between care quality and healthcare payments, more providers have set their sights on implementing vendor-sponsored revenue cycle management solutions that can manage the integration of reimbursement and value.
The healthcare revenue cycle management software and services industry is projected to grow by 15.51 percent between 2014 and 2019, reported Research and Markets in November 2015. As a result of market growth, the total spending on healthcare revenue cycle management solutions is expected to exceed $7.09 billion by 2020, added ReportsNReports.com earlier this year.
More healthcare organizations are seeking outsourced or vendor-created revenue cycle management services to support a range of payment models while the industry transitions, including fee-for-service and value-based reimbursement.
Revenue cycle management solutions include a gamut of services that can help healthcare organizations to optimize and automate business office functions, such as the medical billing process, claims management, eligibility verification, claim denials management, and predictive payment analysis.
But what vendors are topping the charts in this market for the hospital sector? And how does a healthcare organization select the most appropriate revenue cycle management solution?
Using Definitive Healthcare data, RevCycleIntelligence.com explores the most popular revenue cycle management, claims processing, and clearinghouse vendors as well as tips for choosing the best vendor for an organization’s specific needs.
What Is Healthcare Revenue Cycle Management?
Breaking down revenue cycle management solutions
While health IT adoption was nearly universal in 2015 with 96 percent of hospitals reporting certified EHR use, according to the ONC, more providers are now looking to technological solutions to improve revenue cycle management, especially under value-based reimbursement models.
The push for revenue cycle management outsourcing is primarily being driven by declining claims reimbursement rates and the value-based care transition, stated a September Black Book Market Research survey.
Approximately 59 percent of medical providers and 86 percent of hospitals out of the 2,000 independent physician practices and 200 hospitals surveyed stated that their organizations plan to eliminate some revenue cycle management functions, such as medical billing processes, that are resource-intensive, error prone, manual, and back-end by the third quarter of 2017.
The survey also found that about 90 percent of small, independent physician practices also felt that they were not financially or technically prepared for the challenges associated with value-based reimbursement.
Many providers viewed revenue cycle management outsourcing and vendor solutions as a way to make their practices more efficient and for good reason. About 82 percent of practices in the survey that recently outsourced business office functions experienced a decrease in the number of rejected claims and time it takes to collect payments from payers.
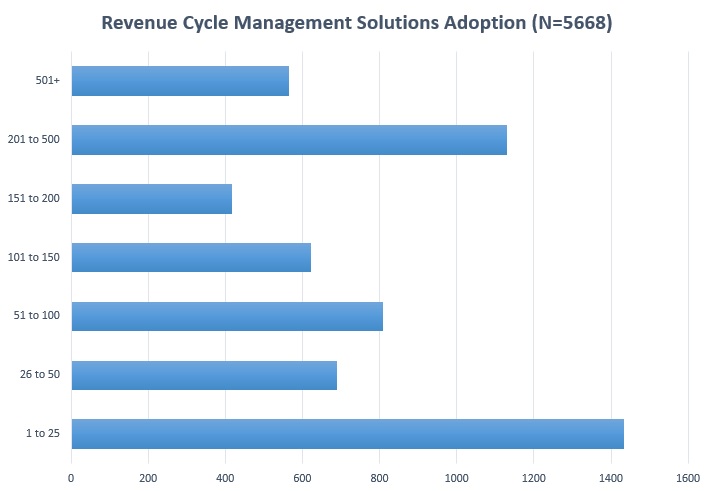
While healthcare organizations are pushing for revenue cycle management solutions, small and large hospitals are leading the way. Out of 5,668 care sites in the Definitive Health database, approximately 25 percent of hospitals with 25 or fewer beds and 20 percent of hospitals with 201 to 500 beds have adopted revenue cycle management solutions.
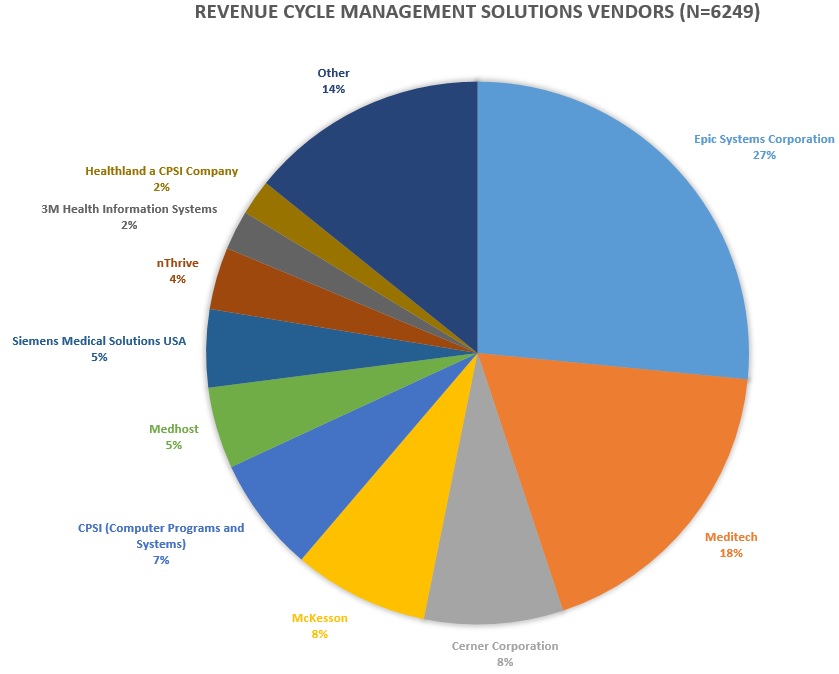
The Definitive Healthcare data also revealed the vendors currently topping the healthcare revenue cycle management space. The data from 6,249 care sites showed that Epic Systems Corporation has the largest market share in revenue cycle management solutions with 27 percent of care sites. Although, MEDITECH is a close second with 18 percent of care sites.
Other top revenue cycle management solutions vendors with more than 100 users included Cerner Corporation (eight percent), McKesson (eight percent), and Computer Programs and Systems, Inc. (CPSI) (seven percent).
Epic Systems Corporation and MEDITECH have maintained their market lead since March 2016, according to Definitive Healthcare data from earlier this year.
However, the healthcare revenue cycle management solutions market may be changing in the next year. Another Black Book Market Research survey from September revealed that 85 percent of provider organizations, hospitals, and physician practices are looking to replace their current systems or deciding if it is time to replace their vendor.
More healthcare professionals are willing to do away with their current revenue cycle management, financial, and coding technology vendors. About 93 percent of 5,000 healthcare leaders said they would switch vendors or systems if an existing product has not generated a return on investment by the end of the year.
Only 79 percent said the same thing in the fourth quarter of 2015, showing an increasing urgency to achieve ROI with these vendor solutions.
Preparing the Healthcare Revenue Cycle for Value-Based Care
Which Healthcare Big Data, Business Intelligence Vendors are Most Popular?
Automating claims processing to optimize healthcare RCM
Claims management is a major revenue driver for healthcare organizations, but about one-third of providers still use a manual versus automated process to manage claims, including denials, reported a July HIMSS Analytics survey.
Out of the providers that have automated claims management processes, only 44 percent reported using a vendor solution, while another 18 percent built an in-house system.
With many healthcare organizations managing a range of payment models, including anything from fee-for-service to full financial risk value-based reimbursement, HIMSS Analytics Director of Research Brendan Fitzgerald stated that “it came as a surprise that more organizations have not automated the denial management process through a vendor-provided solution.”
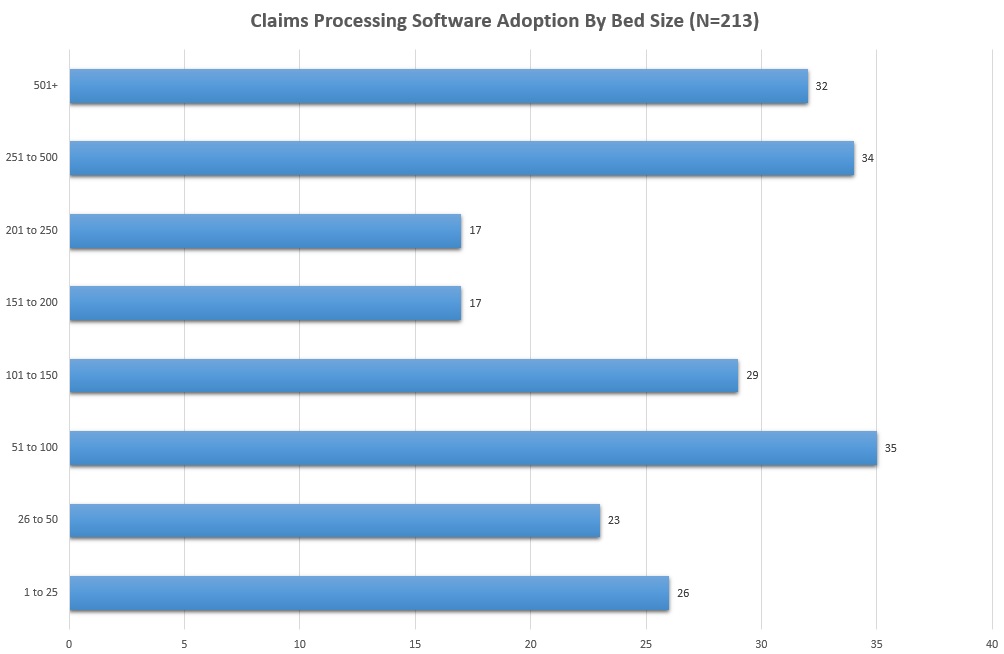
Similarly, Definitive Healthcare data showed that claims processing solutions were not as widely used, especially compared to more general revenue cycle management services. Only 213 care sites have adopted claims processing software, which manages a spectrum of services including multi-payer claim submission, compliance, healthcare fraud prevention, and claim resolution monitoring.
Despite lower adoption rates, claims processing software has been installed across hospitals of all sizes. While more hospitals with 51 to 100 beds implemented the software with 16 percent of total care sites, hospitals of all sizes have similarly invested in the automated claims management tool.
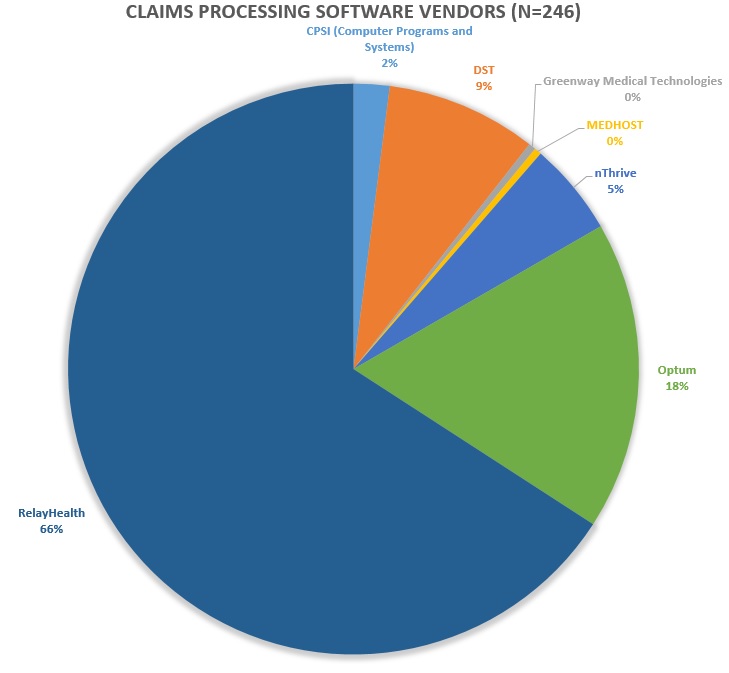
Unlike the revenue cycle management solutions space, though, the claims processing software market was fairly consolidated. Out of the 246 care sites reporting a vendor, 66 percent partnered with RelayHealth.
DST followed with nine percent of care sites, followed by nThrive with five percent, CPSI with two percent, and Greenway Medical Technologies and MEDHOST with less than one percent each.
Even though fewer hospitals outsourced claims management compared to revenue cycle management, a vendor-sponsored claims processing solution may help to optimize claim submissions and reimbursement, Monte Sandler, Executive Vice President of NextGen RCM Services, told RevCycleIntelligence.com in March 2015.
“Because a higher percentage of respondents do billing in house, they lack the benefit of a best practice outsourcer,” said Sandler.
A vendor or automated solution can also help providers to navigate the maze of different payer rules and codes while ensuring the organization complies with claim submission requirements, stated Michelle Tohill, Director of Revenue Cycle Management at Bonafide Management Systems.
“Keeping up with all the diagnostic codes and different insurance policies can be exhausting, but there are many software providers that will automatically update codes and requirements,” explained Tohill. “This cuts down on your research time, allowing your billing team to spend more time double-checking claims to make sure they meet every single requirement.”
How to Maximize Revenue with Improved Claims Denials Management
Key Ways to Improve Claims Management and Reimbursement in the Healthcare Revenue Cycle
Using a clearinghouse vendor to streamline healthcare RCM
Healthcare organizations have a plethora of vendors and services to choose from when it comes to revenue cycle management solutions, including more general management or department-specific services. However, many organizations elect to work with a clearinghouse to maximize claims revenue.
A clearinghouse acts as an intermediary between healthcare providers and payers for claim submission and payment. Providers send billing and claims submission information to the clearinghouse where it is checked for errors, verified for the correct codes, transformed into electronic format, and made compatible with payer software.
While in-house claim denials management software and electronic claims processing solutions currently exist, more hospitals have partnered with a clearinghouse to streamline medical billing and improve revenue cycle management. The HIMSS Analytics survey from July found that 67 percent of healthcare organizations that have outsourced claims management use a clearinghouse vendor solution.
Data from Definitive Healthcare also showed that hospitals are more likely to use a clearinghouse solution rather than other more specific services. For example, only about 150 care sites reported using denials management software and another 86 had electronic claims processing services. But 359 care sites stated that their organization used a clearinghouse vendor.
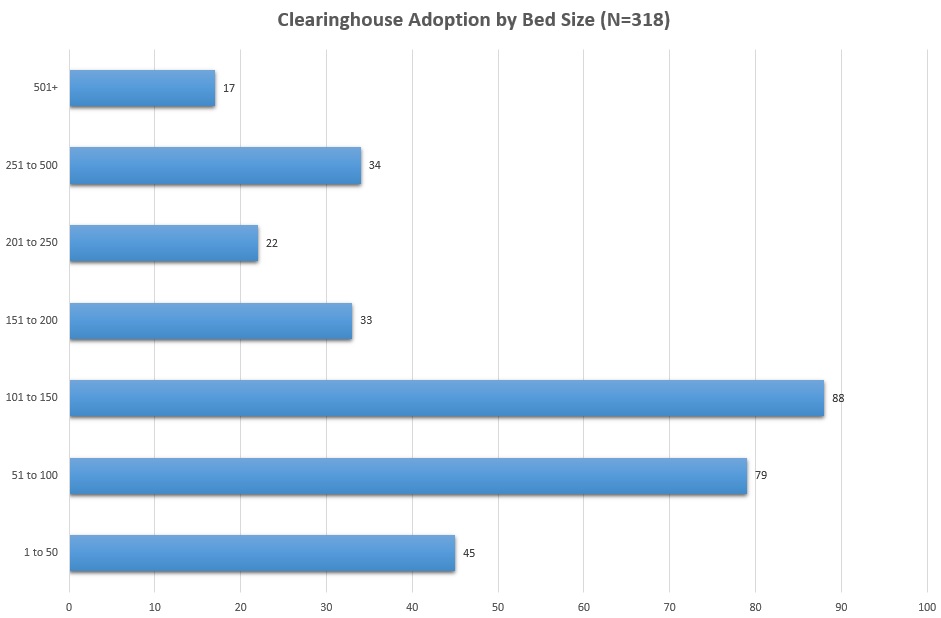
Smaller hospitals were also more likely to partner with a clearinghouse compared to their larger counterparts. Care sites with 150 beds or fewer accounted for about two-thirds of the total facilities using a clearinghouse.
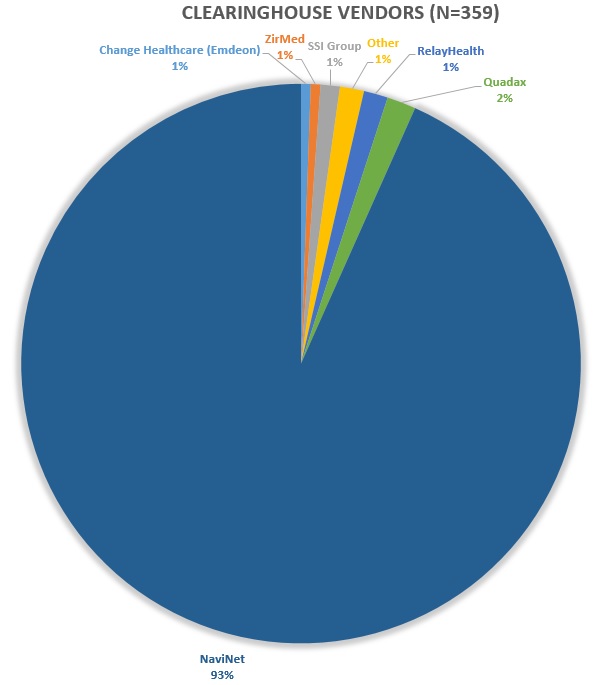
Regardless of number of beds, however, most care sites used NaviNet as a clearinghouse vendor. Approximately 93 percent of all sites partnered with NaviNet.
Quadex followed with just two percent, while Change Healthcare (Emdeon), ZirMed, SSI Group, and RelayHealth held one percent of the market each.
While clearinghouse vendors can help healthcare organizations to transition to electronic claim submissions and cut down on payment cycles, the California Orthopaedic Association urged organizations to ensure that their clearinghouse selection also partners with the same payers and hospital or provider medical billing software is compatible with the vendor’s technology.
4 Medical Billing Issues Affecting Healthcare Revenue Cycle
What Are the Front-End Steps of Revenue Cycle Management?
Considerations for choosing the most appropriate RCM vendor
Deciding on the best revenue cycle management vendor for a healthcare organization can be a daunting task, but revenue cycle leaders should first consider how well they trust a vendor and if there are specialty-specific solutions.
In a story of revenue cycle management lessons learned, Sturdy McKee, San Francisco Sport and Spine Therapy, told RevCycleIntelligence.com in November 2014 that mistrust with vendors almost caused him to forget outsourcing revenue cycle management functions altogether.
McKee explained that a previous vendor for his physical therapy practice only provided a 20 percent collection rate, which strained his operations. The lack of return on investment caused him to feel skeptical with revenue cycle management vendors.
“To be perfectly candid, after our experiences, I was not looking to outsource our billing and the revenue cycle piece,” said McKee. “I mean that was the last thing on my mind and that is part of why we agreed to sign up with a practice management software and pay for it without incorporating the billing because I just didn’t trust anybody.”
McKee finally partnered with a vendor that provided a specialized physical therapy solution. While hospitals may have more vendor options, specialty and smaller practices may want to consider a specialty- or size-specific solution that can better manage the different payer mix and collection challenges.
"[W]e agreed to sign up with a practice management software and pay for it without incorporating the billing because I just didn’t trust anybody."
Healthcare organizations should also understand the costs associated with implementing a vendor solution. A recent peer60 survey found that 83 percent of hospital executives consider cost as the most important criterion in the revenue cycle management vendor decision-making process.
Revenue cycle management solutions will likely never be free. Organizations should think of their budget before implementing vendor solutions. For example, clearinghouses may charge per claim submission, so an organization should be aware of how much they can afford.
The survey also showed that hospital executives tend to get peer opinions on vendors before deciding on one in particular. About 61 percent said peer referrals were a key criterion in the decision-making process.
Additionally, healthcare organizations should consider how involved they want vendors to be in their organization’s revenue cycle management processes. Outsourced solutions can range from just a consulting job to end-to-end outsourcing.
However, about 40 percent of hospital executives prefer to only partner with a vendor for revenue cycle management consulting, followed by co-management with 38 percent, peer60 reported. Only five percent said they wanted to fully outsource revenue cycle management.
While there is a lot to consider when selecting a revenue cycle management vendor, the market is expected to grow and change as new payment models merge. As more providers and payers move to value-based reimbursement, the opportunity for market growth and diversity is projected to increase.
The market opportunities may bode well for healthcare organizations currently transitioning to value-based care, especially under MACRA. From revenue cycle management consulting to end-to-end outsourcing, using technologies that are able to fuse clinical outcomes and clean claims submissions will likely help providers get paid.
Why it’s Important to Select the Right Revenue Management System






