
Christian Delbert - stock.adobe.
The Difference Between Medicare and Medicaid Reimbursement
Medicare and Medicaid reimbursement models vary according to federal and state regulations, but both are striving to embrace value-based reimbursement.
Medicare and Medicaid are government healthcare programs that help individuals acquire coverage, but similarities between the programs more or less end there. Medicare and Medicaid reimbursement structures vary significantly by program and state.
HHS describes Medicare as an insurance program, whereas Medicaid is an assistance program. The federal government offers Medicare coverage to individuals who are 65 years or older, have certain disabilities, and suffer from end-stage renal disease or ALS.
On the other hand, Medicaid is a federal and state-sponsored program that assists low-income individuals with paying for their healthcare costs. Each state defines who is eligible for Medicaid coverage, but the program generally covers individuals who have limited income, including:
- Individuals 65 years or older
- Children under 19 years old
- Pregnant women
- Individuals living with a disability
- Parents or adults caring for a child
- Adults without dependent children
- Eligible immigrants
Depending on the state, Medicaid beneficiaries may pay premiums, deductibles, copayments, and coinsurances to receive coverage. The federal government also funds an average of 57 percent of the operating costs for each state’s Medicaid program based on the state’s Medicaid expenditures.
Meanwhile, the Medicare program is primarily funded through payroll taxes and Social Security income deductions. Beneficiaries are also responsible for a portion of Medicare coverage costs through deductibles for hospital services and monthly premiums for other healthcare services.
Medicare and Medicaid reimbursement models have evolved over the past 50 years, and will continue to do so as value-based care changes the way providers receive payment for their services.
Examining Differences Between Medicare, Medicaid Reimbursement
How Medicare, Medicaid, and CHIP Guide the Health Payer Industry
The A, B, C, and Ds of Medicare reimbursement
CMS divides Medicare coverage into four parts, each with their own claims reimbursement structures. Medicare Parts A and B are considered “traditional Medicare” and cover inpatient and outpatient services, whereas Part C includes Medicare Advantage plans and Part D covers prescription drugs.
Traditional Medicare reimbursement
Approximately two-thirds of Medicare’s benefit spending stems from services performed by providers in traditional Medicare.
The providers who receive traditional Medicare reimbursement range from hospitals, physicians, post-acute care facilities, and hospice agencies to durable medical equipment suppliers, ambulance providers, and laboratories. Medicare reimburses each provider type using separate payment rates and systems.
However, traditional Medicare reimbursement generally falls into two categories: Part A services and Part B services.
Medicare Part A services include inpatient hospital, skilled nursing facility, nursing home, hospice, and home health care. Providers primarily receive Medicare reimbursement for the hospital-based services under the inpatient prospective payment system (IPPS).
Under the IPPS, hospitals receive a prospective payment per beneficiary discharge. CMS determines the rate based on one of over 700 Diagnosis Related Groups (DRGs), which adjust payments according to patient age, sex, secondary diagnosis, and services received.
CMS assigns each DRG a payment weight by establishing a benchmark for the average resources used to treat a Medicare beneficiary with that diagnosis. DRGs that require more intense care or longer lengths of stay receive higher base reimbursement rates.
The federal agency then multiples the DRG payment weight by the average price per case for all Medicare cases in that year. The amount includes a labor-related component that adjusts for the area’s wage index and a non-labor component that accounts for the hospital’s geographic location in an urban or rural area.
Some hospitals also receive supplemental Medicare reimbursement under the IPPS. If a hospital treats a high percentage of low-income patients, Medicare pays the facility an add-on payment, known as the Disproportionate Share Hospital adjustment.
Medicare also increases IPPS rates for teaching hospitals and individual outlier cases that generate unusually high healthcare costs.
In addition, hospitals may be subject to value-based reimbursement adjustments under the IPPS. Qualifying hospitals face value-based penalties or incentive payments through the following IPPS programs:
- Hospital Value-Based Purchasing. Value-based penalties or incentive payments are subject to hospital performance on clinical care, patient and caregiver experience of care coordination, patient safety, and efficiency and cost reduction.
- Hospital-Acquired Condition Reduction Program. This program penalizes hospitals in the worst-performing quartile for their inability to significantly reduce hospital-acquired conditions.
- Hospital Readmissions Reduction Program. Hospitals with excessive 30-day readmission rates will see their IPPS payments reduced up to 3 percent.
Medicare Part B covers outpatient and physician-based ambulatory services. Providers furnishing the services primarily receive Medicare reimbursement via the hospital outpatient prospective payment system (OPPS) or the Physician Fee Schedule.
CMS pays hospitals where Medicare Part B beneficiaries receive outpatient care under the OPPS. The federal agency sets OPPS reimbursement rates using the Ambulatory Payment Classifications (APCs), a package of similar services based on clinical factors and costs. The federal agency identifies the services using Healthcare Common Procedure Coding System (HCPCS) codes.
Each APC receives a scaled relative payment weight that represents the average healthcare costs for the services included in the package. Then, the weight is multiplied by a conversion factor to create a national unadjusted payment rate.
CMS also adjusts OPPS rates by the hospital wage index to offset geographical variations in healthcare costs.
However, some hospital outpatient services are paid separately from an APC. Some hospital outpatient services do not belong to an APC, such as surgical, diagnostic, and non-surgical therapeutic procedures, blood and blood products, most clinic and emergency department visits, certain preventative services, and some drugs.
CMS establishes unique reimbursement structures for these outpatient services. For example, hospitals would generally receive the average sales price plus a percentage of the cost for prescription drugs.
The federal agency also reimburses partial hospitalizations on a per diem basis. Medicare reimbursement rates depend on the number of individual services provided to the patient in one day.
Similar to its hospital inpatient counterpart, the OPPS also provides some hospitals with add-on payments. The Medicare reimbursement system includes pass-through payments for certain drugs, biologicals, and devices as well as add-on payments for outlier cases, cancer hospitals, and rural facilities.
Medicare Part B also covers physician services and reimburses providers for over 7000 items via the Physician Fee Schedule.
These services include office visits, surgical procedures, anesthesia services, and other diagnostic and therapeutic procedures. Providers can also bill Medicare under the Physician Fee Schedule for services provided in a range of settings, including hospitals, physician offices, ambulatory surgical centers, post-acute care settings, and patient homes.
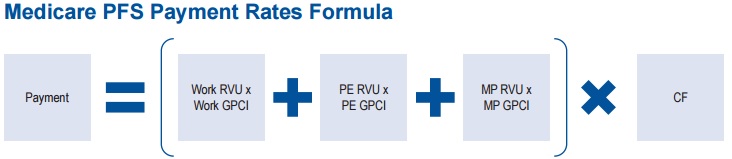
Medicare Physician Fee Schedule rates use relative value units (RVUs) to set reimbursement amounts. CMS uses the following RVUs to determine the rates:
- Work RVU: relative time and intensity related to furnishing services to Medicare patients
- Practice Expense RVU: costs of maintaining a practice, such as renting space, buying supplies and equipment, and staffing
- Malpractice RVU: cost of malpractice insurance
Then, the federal agency adjusts the three RVU values for geographic cost variations using Geographic Practice Cost Indices. The sum of the adjusted RVUs is then multiplied by a conversion factor determined by Congress each year.

CMS updates the Physician Fee Schedules rates each year to reflect accurate healthcare costs by geographic region.
Part C and D reimbursement
Medicare Part C strays from traditional Medicare because private companies manage enrollee benefits and provider claims reimbursement. Part C is also known as Medicare Advantage.
One in three Medicare beneficiaries has enrolled in Medicare Advantage because the plans offer additional coverage. Some Medicare Advantage plans offer prescription drug, vision, and dental coverage that is not available under basic Medicare policies.
The federal government also requires Medicare Advantage plans to cap out-of-pocket spending, unlike traditional Medicare. Under traditional Medicare, beneficiaries pay a portion of the healthcare costs for each service. But Medicare Advantage plans include an out-of-pocket spending maximum. Once beneficiaries hit the limit, all services are covered.
Medicare reimburses Medicare Advantage plans with a capitated amount per beneficiary for Part A and B benefits. CMS determines capitated amounts in each area through a bidding process. Plans submit bids to the federal agency that reflect the estimated healthcare costs per beneficiary for the covered services.
Bids that meet CMS standards are accepted and compared to a regional benchmark. The benchmark represents the maximum amount Medicare will pay a plan in a region. If a plan’s bid is higher than the benchmark, beneficiaries must make up the difference. Plans with bids lower than the benchmark must use the additional funds to provide supplemental benefits.
By 2017, CMS plans to alter benchmark values to account for 95 percent of traditional Medicare costs in the areas with the greatest per capita Medicare costs. The benchmark will account for 115 percent of traditional Medicare costs in low-cost areas.
With the capitated payments, Medicare Advantage plans reimburse providers through individual contracts. Each contract contains its own payment structure, ranging from fee-for-service or risk-based alternative payment models.
Most Medicare Advantage enrollment in 2016 (64 percent) fell under a health maintenance organization (HMO), Kaiser Family Foundation reported.
The second most common plan by enrollment was a local provider preference organization (PPO) with 23 percent of enrollees, followed by a regional PPO with 7 percent of enrollees.
Fee-for-service structures only represented 1 percent of Medicare Advantage enrollment in 2016.
In a similar fashion, Medicare Part D differs from traditional Medicare because it uses private drug plans to manage voluntary prescription drug benefits. Part D plans supplement either traditional Medicare or Medicare Advantage coverage.
CMS also pays plan sponsors a capitated per-member, per-month payment for benefits management.
However, plan sponsors partner with pharmacies to deliver benefits. Providers typically do not submit claims to Part D plans. Most prescription drugs requiring a provider to submit a claim would be included under Part B.
Medicaid, Medicare Reimbursement $57.8B Below Hospital Costs
Key Ways to Improve Claims Management and Reimbursement in the Healthcare Revenue Cycle
Medicaid reimbursement varies by state
The greatest difference between Medicare and Medicaid reimbursement structures is that each state controls its own Medicaid program. Consequently, every Medicaid program differs based on state regulations.
However, most Medicaid reimbursement models use fee-for-service, managed care, or a combination of both to pay providers.
Fee-for-service payment dominates Medicare reimbursement structures across states. Over one-half of Medicaid spending in 2015 stemmed from a fee-for-service payment model, the Medicaid and CHIP Payment and Access Commission (MACPAC) reported.
Fee-for-service Medicaid reimbursement models pay providers by the volume of services they provide to beneficiaries. States establish their Medicaid reimbursement rates under fee-for-service models, but policymakers must base the rates according to the following federal methodologies:
- Healthcare costs associated with providing services
- Review of commercial payer rates
- Percentage of what Medicare reimburses for equivalent services
Most Medicaid fee-for-service methodologies set rates by the charge for services or maximum allowable price, whichever is lesser. Thirty-eight out of the 51 US Medicaid programs using this method, a recent MACPAC report showed.
In contrast to a fee schedule, states pay providers based on either a percentage of Medicare payment, a state-determined market assessment, or a relative value scale.
Medicaid fee-for-service rates tend to be significantly lower than Medicare reimbursement for similar services. The Kaiser Family Foundation found that Medicaid rates in 2014 were just two-thirds the amount of equivalent Medicare payments.
Fee-for-service currently drives Medicaid spending, but most beneficiaries are enrolled in a managed care plan. CMS reported that 72 percent of Medicaid beneficiaries belonged to some type of managed care plan in 2013.
Under these plans, states contract managed care organizations to handle enrollee benefits and claims management. The plans can contain fee-for-service structures for provider reimbursement, resulting in Medicaid fee-for-service spending increases.
However, they can also include varying levels of financial risk or value-based reimbursement.
Medicaid managed care models generally fall into three categories. First, some states use a comprehensive risk-based managed care model in which plans receive a capitated rate for Medicaid-covered services.
The fixed amount per-member, per-month aims to cover a specific set of services for the beneficiary. However, the plans assume the financial risk if care exceeds the capitated amount.
Providers under the comprehensive risk-based managed care model can be paid via fee-for-service or share in the model’s financial risk arrangements.
In 2013, about 54 percent of Medicaid beneficiaries received care under a plan that included comprehensive risk-based managed care, MACPAC reported.
Limited benefits plans are also common, covering 49.5 percent of beneficiaries. States with this managed care option partner with limited benefits plans to provide services for specific patient populations or to manage certain benefits.
The limited benefits plan may hone in on specific services, such as inpatient mental health, non-emergency medical transportation, oral health, or chronic disease management.
Third, a small portion - 12.7 percent - of Medicaid beneficiaries fall under primary care case management models. Primary care providers serving these beneficiaries receive a monthly case management fee.
States intend for the primary care provider to use the care management fee to manage and coordinate basic medical care for each beneficiary. Providers are still reimbursed via fee-for-service and the plan absorbs the financial risk.
Do Medicaid Reimbursement, Admissions Produce Hospital Profit?
FFS, Risk-Based Medicaid ACO Programs Similarly Reduce Costs
The evolving Medicaid and Medicare reimbursement landscape
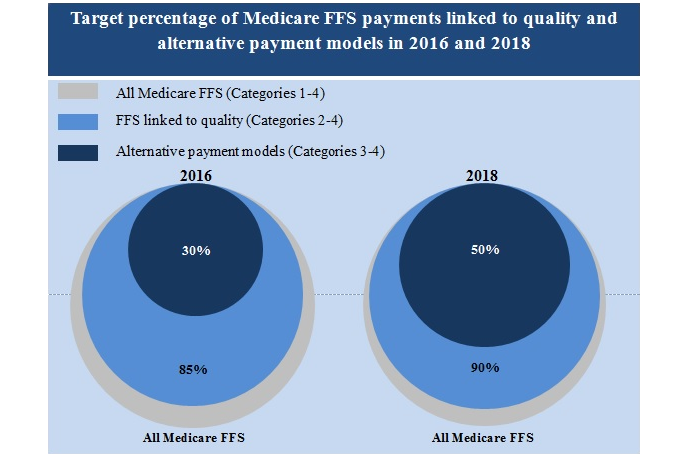
HHS has announced explicit goals to tie most of its traditional Medicare payments to value-based reimbursement models. Healthcare leaders intend to link one-half of Medicare reimbursement to an alternative payment model by 2018.
They also anticipate shifting 90 percent of traditional Medicare payments to a quality-based structure by the same time.
HHS has started the shift away from fee-for-service payments through some of its IPPS programs, such as the Hospital Readmissions Reduction and Hospital Value-Based Purchasing models.
Healthcare leaders and lawmakers recently took a substantial step toward value-based reimbursement with MACRA. The regulation, passed in October 2016, established the Quality Payment Program.
Under the Quality Payment Program, eligible clinicians can earn value-based incentive payments or be subject to financial penalties. The program will impact Medicare reimbursement starting in 2019 through the Merit-Based Incentive Payment System (MIPS) or the Advanced Alternative Payment Model (APM) track.
HHS expects most eligible clinicians to start Quality Payment Program participation through MIPS. Clinicians will receive a composite performance score based on care quality, specific Improvement Activities, the technology component of Advancing Care Information, and cost.
Based on their MIPS composite scores, clinicians will see their Medicare reimbursement adjusted upward or downward. The maximum adjustment in 2019 is 4 percent, but HHS intends to ramp up the adjustment to 9 percent by 2022.
Eligible clinicians can also earn the maximum incentive payments by participating in an Advanced APM. Clinicians who partake in one of the seven alternative payment models will face more financial risk compared to their peers in MIPS.
By sufficiently engaging with the risk-based alternative payment models, clinicians will see an automatic 5 percent upward Medicare reimbursement adjustment in 2019.
Healthcare leaders and state policymakers are also jumping on board with value-based reimbursement for Medicaid payments.
A recent National Association of Medicaid Directors (NAMD) survey revealed that value-based reimbursement reform topped the 2017 priority list for Medicaid directors. Eight states also identified delivery system payment reform as one of their long-term strategic priorities until 2021.
A number of states have also implemented value-based reimbursement models. For example, 10 states currently manage Medicaid accountable care organizations (ACOs) with some successes, a recent NAMD report stated. Colorado’s Medicaid program saw $77 million in net savings under its ACO programs and Minnesota’s Integrated Health Partnerships ACO program saved $76.3 million.
Medicaid programs are also realizing cost savings through high-quality care and reduced healthcare utilization. Oregon’s Medicaid ACO initiative decreased emergency department visits among members by 23 percent.
Based on Medicaid ACO results, 11 more states plan to develop similar shared savings or global budget ACOs, a recent NAMD report stated.
Medicaid and Medicare programs may face more changes than commercial claims reimbursement models because of government control. The recent presidential election brought many political concerns to light with the healthcare programs.
From a potential Affordable Care Act repeal to possible Medicaid block grant funding, policymakers are scrutinizing the federal programs to improve care quality for beneficiaries while lowering healthcare costs.
However, the shift away from fee-for-service is seemingly here to stay and providers should anticipate both Medicare and Medicaid reimbursement to increasingly fall under alternative payment models.






