
Getty Images/iStockphoto
Overcoming Rural Hospital Revenue Cycle Management Challenges
Rural hospitals face many unique revenue cycle management challenges, including health IT and value-based care.
Despite serving as a critical healthcare safety net for millions of patients, many rural hospitals are constantly on the brink of closing their doors due to a number of revenue cycle management challenges.
Eighty-two rural hospitals have closed since 2010, and many more are considering shutting down because of low operating margins, challenging patient populations, and provider shortages.
In 2016, 41 percent of rural hospitals operated with negative margins. As patient populations get older, regulatory programs become more challenging, and resources remain scarce, stakeholders fear that the safety net may be unraveling.
What makes revenue cycle management more difficult in the rural hospital setting? And how can these organizations overcome key operational challenges stemming from their unique position?
The unique position of rural hospitals
Patient characteristics heavily influence rural hospital revenue cycles. Residents in rural regions are more likely to experience socioeconomic and clinical challenges, resulting in higher costs.
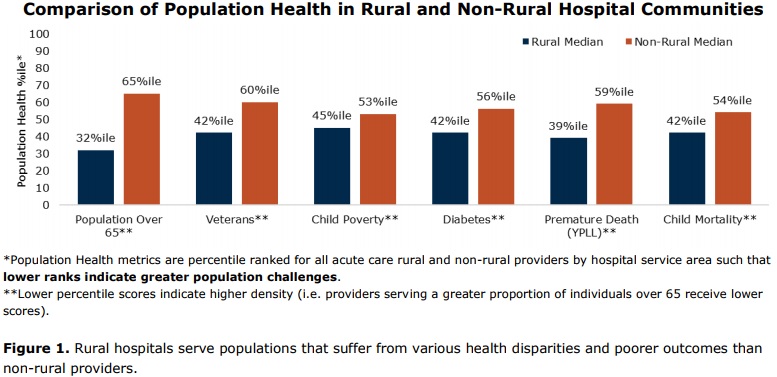
A recent study showed that rural hospitals overwhelmingly treat more patients who are over 65 years old, more veterans, and larger numbers of diabetics than their non-rural peers. Their patients are also significantly more likely to experience childhood poverty, premature death, and increased childhood mortality rates.
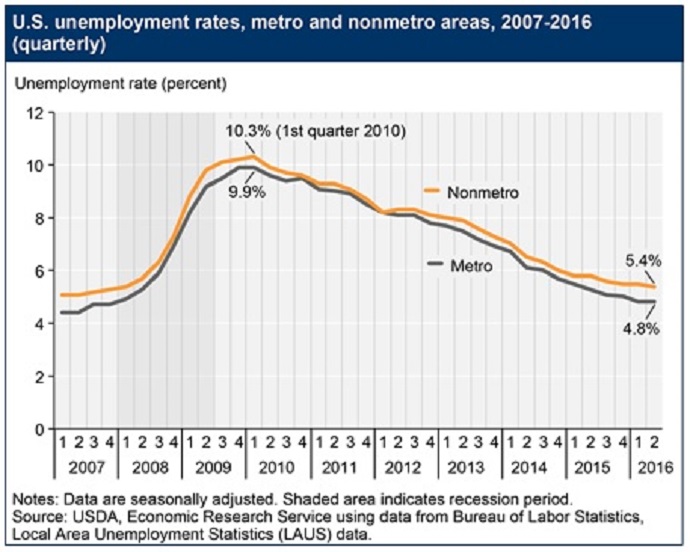
Rural areas also consistently witness higher unemployment rates. The unemployment rate in non-metro areas reached 5.4 percent halfway through 2016, while metro regions reported an average rate of 4.8 percent, the US Department of Agriculture reported.
With fewer employed residents, employer-sponsored health plans account for a smaller portion of rural hospital payer mix, and uninsured patients unable to afford health insurance coverage are common.
As a result, hospitals experience more difficult negotiations with private payers and do not have the same leverage as facilities in densely populated regions to negotiate higher claims reimbursement rates.
Making matters worse, leaders from several hospitals that closed in rural areas reported that the small share of privately insured patients in their communities tended to seek care at newer, larger hospitals within a reasonable distance from the rural hospital, according to a recent Henry J. Kaiser Family Foundation report.
Consequently, many rural hospitals rely heavily on Medicare and Medicaid to cover patient care costs - but reimbursement rates from public insurers were $57.8 billion below actual spending in 2015.
Rural Hospitals the ‘Lifeblood’ of the Community
Overcoming the challenges of physician shortages
The healthcare industry as a whole is facing a serious physician shortage problem. The American Academy of Medical Colleges recently estimated the nationwide physician shortage will reach up to 104,900 providers by 2030.
The shortfall spells trouble for rural hospitals already experiencing staffing challenges while treating some of the sickest patient populations. Even though 20 percent of the US population lives in a rural region, only 10 percent of physicians practice in those regions, former CMS Administrator Andy Slavitt reported at the federal agency’s 2016 Rural Health Summit.
The physician shortage in rural areas accounted for 65 percent of the healthcare professional shortage, he added.
Providers are hesitant to set up shop in sparsely populated areas. Just 1 percent of providers in their final year of residency training preferred to work in a community of 10,000 individuals or less. Only 3 percent stated they would practice in a community with fewer than 25,000 residents, a recent Merritt Hawkins survey showed.
Medical residents explained that they did not want to be on a “clinical island” without specialty support, health IT access, and other resources. The lack of shift coverage also played a part in residents’ preferences for larger communities.
Offering higher compensation rates and financial incentives to attract and retain providers may not be a viable option for rural hospitals already operating under negative margins.
Therefore, rural hospitals should alleviate physician shortages and minimize their costs by implementing team-based care models that depend on advanced practice clinicians.
A 2016 case study in the Journal of Clinical Outcomes Management found that hospitalist care teams that used a higher physician assistant-to-physician ratio reduced care costs more than other teams in the same hospital that used a traditional staffing model.
Care teams with more physician assistants incurred expenses that were 3.52 percent less than the care expenses under the other team.
Healthcare organizations that boosted their advanced practice clinician workforce also reported greater productivity, a recent MGMA survey added. Practices with greater numbers of advanced practice clinicians experienced a 34 percent boost in productivity compared to their peers.
By managing daily responsibilities and prepping patients, advanced practice clinicians allow physicians in rural hospitals to focus on more complex cases and higher priority tasks.
Not only do advanced practice clinicians maximize operating costs and productivity, but the non-physician staff members cost less to employ.
For example, median annual compensation for physician assistants was $102,000 in 2016, compared to the average salary of $195,000 for a primary care physician.
While physicians are still needed at rural hospitals, broader care teams can help to relieve pressure on organizations to fill open physician roles. However, leaders should be aware of state laws that may prohibit advanced practice clinicians from engaging in specific services or procedures without physician supervision.
Medical Resident Shortage Hinders Rural Patient Care Access
Partnerships with Hospitals, Clinics Up Rural Patient Care Access
Maximizing limited capital for health IT investments
Like other industries, healthcare is embracing technology to improve quality, productivity, and spending. Using automated systems to monitor patient outcomes and costs, as well as link clinical and financial data, is key to maximizing reimbursement, especially under value-based care models.
However, rural hospitals may be left behind when it comes to health IT implementation because tighter operating budgets prevent investment in new systems and upgrades.
In 2015, a typical health IT implementation cost practices up to $32,500 per physician, MGMA reported. This represents a 40 percent increase since 2011. Costs included IT equipment, staff, maintenance, and other expenses.
As a result, many rural hospitals are still stuck in the “dark ages,” stated Brad Huerta, the CEO of a frontier and critical access hospital in Idaho. When he first started his position at Lost Rivers Medical Center, the facility did not even have Wi-Fi.
The hospital’s remoteness meant that Lost Rivers Medical Center did not have the revenue or staff to spare for health IT implementation projects. But Huerta knew that embracing technology was the only way to remain open and independent.
Paper-based processes detracted from provider productivity and made it more difficult for hospital leaders to identify revenue cycle improvement opportunities, he said, especially with insufficient access to current and complete financial and clinical data.
To improve his hospital’s revenue cycle while minimizing health IT costs, Huerta invested in cloud-based technologies, including an EHR system.
“To be able to have a completely web-based system meant I didn’t have to hire an army of IT guys and I didn’t have to have a server farm in my hospital,” he explained.
“The only thing harder for a critical access hospital to recruit other than a doctor is an IT guy. For us, it made sense from the operational side, but it also made financial sense.”
Using cloud-based health IT systems, providers shaved two to three hours off the time they needed to dedicate to administrative tasks. The ability to chart in the exam room with a computer instead of on paper after the appointment also allowed providers to capture charges in real-time.
The hospital no longer left money on the table. Total cash flow improved by 119 percent and days in A/R decreased from over 100 days to around 52.
EHR Adoption, Population Health a Struggle for Rural Providers
Reducing uncompensated care and bad debt
Medicare and Medicaid payment shortfalls and higher rates of uninsured patients compound uncompensated care costs and patient bad debt at rural hospitals.
Charity care and patient bad debt represented almost 6 percent of rural hospital budgets compared to just 5.1 percent of urban hospital expenses, a 2015 Flex Monitoring Team report showed. Critical access hospitals particularly struggled with the economic burden of uncompensated care, with charity care and patient bad debt comprising 7.4 percent of their total expenses.
CMS aims to support rural hospitals and other organizations with high uncompensated care costs through cost-based reimbursement for critical access hospitals. Medicare and Medicaid also offer federal Disproportionate Share Hospital payments, which provide supplemental reimbursements to hospitals that treat greater portions of Medicaid and uninsured patients.
However, rural hospitals still experience payment shortfalls from claims reimbursements that do not cover the cost of total care.
Patients are expected to pay a portion of their costs out of their own pockets. But high poverty and unemployment rates often mean that rural hospitals never see patient financial responsibility paid in full.
About 68 percent of patients with medical bills of $500 or less did not fully pay their medical bills to hospitals in 2016, according to a recent TransUnion Health study.
Implementing flexible payment plans is one strategy that helped a small hospital in Missouri work with their patients to collect the full amount listed on medical bills.
Excelsior Springs Hospital started offering zero percent APR payment plans to their patients in April 2017.
“We don’t want our patients to have to choose between paying for food or rent and healthcare,” said Nanette Houck, the hospital’s interim CEO. “We also want them to have the best care and have a partnership with a company who offers payment plans makes us feel like we are giving our patients options. It helps to take one other stress away from an already stressful healthcare situation.”
Rather than intimidating her patients with a $2000 bill, Houck and her providers gave patients the option to pay off their medical bills in six to 48 months. In extreme cases, payment plans lasted for 70 months.
Houck anticipates that patients will be more willing to pay off medical bills in smaller payments, resulting in additional revenue the hospital may never have seen if not for the payment plans.
Key Ways to Boost Collection of Patient Financial Responsibility
How a Small Hospital Increased Patient Collections by 300%
Succeeding with value-based reimbursements
Value-based reimbursement brings a new batch of revenue cycle management challenges for small and rural hospitals, the Government Accountability Office (GAO) recently reported.
Downside financial risk models require organizations to repay all or some of the financial losses incurred. But the GAO stated that “practices need either to have financial reserves to cover instances such as patients with unexpectedly costly medical events or to purchase reinsurance to cover such expenditures.” Small and rural hospitals tend to have few or none of the requirements.
Dispersed patient populations also impeded small and rural hospitals from implementing effective population health management programs required for value-based reimbursement success.
“Practices’ ability to manage care of their entire patient population is affected by patients’ geographic location and preferences, and this is especially true for rural physician practices whose patients may have to travel distances to receive regular wellness visits and seek specialists when recommended,” wrote the GAO.
To prevent value-based reimbursement issues, rural hospitals should start the transition away from fee-for-service reliance as soon as possible. The National Rural Health Resource Center suggests that rural hospitals step into the value-based reimbursement realm by creating a transition strategy.
The transition strategy should include the following elements:
- Expand primary care services and hours
- Build a larger primary care network as well as align primary care physicians with other providers, foster relationships between departments and staff, create affiliations with neighboring healthcare organizations, and establish a care coordination plan with community partners
- Market care quality and patient satisfaction scores to increase competitive edge
- Continue to maximize fee-for-service revenue by building on existing services and customer loyalty, like marketing services to local providers for referrals, offering specialist and acute care services based on community needs, and marketing swings beds, imaging, laboratories, and rehabilitation services to increase referrals
- Invest in facilities and health IT
- Engage leadership with transition
Rural hospitals should also start to track key performance indicators (KPIs) that drive value-based reimbursement performance, the National Rural Health Resource Center advised.
The top KPIs rural hospitals should monitor as the organization shifts to value-based reimbursement include:
- Days in net accounts receivable, with favorable values below 52.46 days
- Days in gross accounts receivable, below 50.37 days
- Days cash on hand, above 76.26 days
- Total margin, above 3.09 percent
- Operating margin, above 1.79 percent
- Debt service coverage ratio, above 2.89
- Salaries to net patient revenue, below 44.68 percent
- Payer mix percentage, favorable values for inpatient payer mix below 73.24 percent
- Average age of plant (buildings and equipment), below 10.18 years
- Long-term debt to capitalization, below 27.72 percent
Additionally, rural hospitals should establish emergency department KPIs that primarily track utilization and admission rates. Value-based reimbursement hinges on sending patients to the appropriate setting at the right time to reduce costs.
Using these strategies to become a competitive healthcare innovator with growing operating margins is not impossible for rural hospitals - if leaders invest in their staff, patients, health IT systems, and value-based care.
Pay-for-Performance Models Hurt Safety-Net Hospital Finances






