
Understanding Serotonin and Norepinephrine Reuptake Inhibitors (SNRIs)
SNRIs play a critical role in managing psychiatric and pain disorders, with comparable effects to SSRIs.
Although most people think of selective serotonin reuptake inhibitors (SSRIs) when discussing antidepressants, serotonin and norepinephrine reuptake inhibitors (SNRIs) also play a critical role in managing major depressive disorder and other psychiatric and pain conditions. LifeSciencesIntelligence explores the complex role of SNRIs in healthcare and compares them to SSRIs.
What Are SNRIs?
According to the Mayo Clinic, SNRIs are a class of antidepressants used to manage psychological disorders, including anxiety, depression, and more. This class of medications can also be used to manage chronic pain. This dual action mechanism is thought to provide additional benefits in terms of symptom relief, especially for individuals who may not respond well to SSRIs alone.
By inhibiting the reuptake of serotonin and norepinephrine in the brain, they increase the levels of these neurotransmitters, which help regulate mood, emotions, and other psychiatric functions.
SNRIs are often prescribed when other types of antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs), have not been effective. They can help manage symptoms of depression, generalized anxiety disorder, social anxiety disorder, and other conditions.
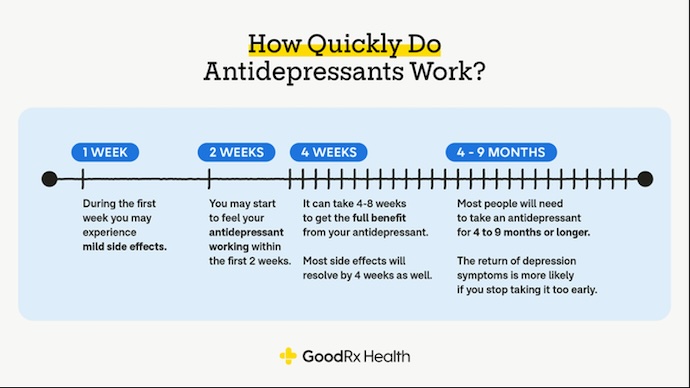
Below is a graphic by GoodRx that outlines the efficacy timeline for antidepressants, including SNRIs. On average, SNRIs take 6–8 weeks to begin working, similar to SSRIs.
SNRIs can be used in combination with other treatment modalities for depression and anxiety. This may include psychotherapy, cognitive behavioral therapy (CBT), or other necessary medications. Combining different approaches can provide a more comprehensive and tailored treatment plan.
Types of SNRIs
According to the GoodRx article, the first SNRI was approved in the United States in 1993, and the most recent was in 2013. There are four FDA-approved SNRIs indicated for depression:
- Desvenlafaxine (Pristiq)
- Duloxetine (Cymbalta):
- Levomilnacipran (Fetzima)
- Venlafaxine (Effexor XR):
Beyond depression, duloxetine is approved for generalized anxiety disorder (GAD), diabetes-related neuropathy pain, fibromyalgia, and chronic musculoskeletal pain. Venlafaxine is also indicated in GAD, social anxiety disorder, and panic disorder.
Beyond the indicated uses, the Cleveland Clinic notes that some healthcare providers prescribe SNRIs off-label to manage other anxiety disorders, menopause-related hot flashes and night sweats, chemotherapy-related peripheral neuropathy, urinary incontinence, attention-deficit/hyperactivity disorder (ADHD), obsessive–compulsive disorder (OCD), and migraines.
Milinacipran is another SNRI; however, it is only FDA-approved for patients with fibromyalgia.
According to an article in CNS Spectrums, SNRIs block serotonin and norepinephrine at different levels. Duloxetine blocks serotonin at a 10 times greater level than norepinephrine. Venlafaxine has a 30 times greater affinity for serotonin than norepinephrine.
Researchers in StatPearls note, “In contrast with other selective serotonin–norepinephrine reuptake inhibitors like duloxetine, venlafaxine, and desvenlafaxine; milnacipran and levomilnacipran have a higher selectivity for inhibiting norepinephrine reuptake than serotonin reuptake.”
Dosing
StatPearls provides dosage information on SNRIs. For venlafaxine, providers typically start by prescribing 75 mg daily and increasing the dose as needed. On average, patients achieve maintenance at 225–375 mg daily.
Patients on desvenlafaxine start at 25–50 mg daily and usually achieve maintenance at 50 mg daily. The starting daily dose for duloxetine is 30 mg, but the average maintenance dose is 60 mg.
Milnacipran prescriptions start at 12.5 mg daily, and most patients end up taking 100 mg. Finally, levomilnacipran prescriptions begin at 20 mg daily, and patients’ maintenance doses can vary dramatically from 40 to 120 mg daily.
Common Side Effects
There are multiple risks associated with SNRIs, as with any antidepressant or psychiatric medication. Less serious risks include common side effects. Potential side effects include nausea, dry mouth, dizziness, headaches, and excessive sweating. Other side effects may include fatigue, constipation, insomnia, sexual dysfunction, and appetite loss.
“Tolerability of an SNRI at therapeutic doses varies within the class. Although no direct comparative data are available, venlafaxine seems to be the least well-tolerated, combining serotonergic adverse effects (nausea, sexual dysfunction, withdrawal problems) with a dose-dependent cardiovascular phenomenon, principally hypertension. Duloxetine and milnacipran appear better tolerated and essentially devoid of cardiovascular toxicity,” researchers in the CNS Spectrums article stated.
Generally, the side effects of SNRIs are inconsequential compared to the potential risks of untreated psychiatric disorders. For most patients, the side effects resolve within a few weeks of treatment.
However, there are more serious potential complications, including the following:
- Suicidal thoughts or behavior
- Serotonin syndrome
- Antidepressant discontinuation syndrome
Suicidal Thoughts and Behaviors
People under 25 who take SNRIs may be at an increased risk of suicidal thoughts or ideations. The highest risk is at treatment initiation or when their prescriber changes their dosage.
Serotonin Syndrome
Beyond suicidal thoughts and behaviors, serotonin syndrome, caused by excess levels of serotonin, can be a fatal condition. Although this is a rare side effect, SNRIs taken alongside other medications that increase serotonin levels can trigger serotonin syndrome. The condition can cause nervousness, nausea, vomiting, diarrhea, dilated pupils, involuntary muscle contractions, spasms, rigidity, sweating, shivering, and side-to-side eye movements.
Beyond that, more severe symptoms of serotonin syndrome include confusion, delirium, tachycardia, high blood pressure, fever, seizures, and loss of consciousness.
Antidepressant Discontinuation Syndrome
Finally, antidepressant discontinuation syndrome, or SNRI withdrawal, can cause the following side effects:
- Flu-like symptoms, including fatigue, headache, achiness, and sweating
- Insomnia
- Nausea
- Dizziness or lightheadedness
- Sensory issues
- Anxiety
- Irritability or agitation
Although some people may refer to this condition as SNRI withdrawal, it is not technically classified as withdrawal because these drugs are not addictive; however, patients who suddenly discontinue SNRIs after taking them for six or more weeks may have withdrawal-like symptoms.
Contraindications
While SNRIs can be effective in treating depression and anxiety, they may not be suitable or effective for everyone. The decision to use SNRIs or any other medication should be made in consultation with a healthcare professional who can assess a patient’s needs and provide personalized recommendations. For some patients, there are contraindications for SNRI use.
In some cases, venlafaxine, levomilnacipran, and desvenlafaxine can increase blood pressure, which means hypertensive disorders are a contraindication for their use.
Alternatively, hypertensive patients who need SNRIs may be prescribed duloxetine. However, that comes with its own set of side effects, worsening existing liver problems.
Some compounds that may impact SNRI efficacy and compromise patient safety include other antidepressants or St. John’s wort — which elevate serotonin levels — nonsteroidal anti-inflammatory drugs (NSAIDs), medications that cause bleeding, and alcohol.
How Do SNRIs Compare to SSRIs?
SNRIs are considered dual-action antidepressants because they affect both serotonin and norepinephrine, whereas SSRIs primarily target serotonin.
Unlike SSRIs, “SNRIs seem to be helpful in relieving chronic pain associated with and independent of depression,” noted researchers in the CNS Spectrums article.
In an article published in the Journal of Clinical Pharmacy and Therapeutics, researchers compared the efficacy of SSRIs and SNRIs for managing major depressive disorder by analyzing 25 studies gathered from multiple sources.
According to the study, SNRIs are 27% more effective than SSRIs. Based on the meta-analysis, remission rates for SNRIs were 48.5%, while for SNRIs they were 41.9%. However, more patients on SNRIs discontinued medication due to adverse drug reactions, with a 3.2% greater rate.
“SNRIs showed statistical but not clinical significance when compared with SSRIs in treating MDD,” concluded researchers in the publication.




