
metamorworks/istock via Getty Im
Understanding Good Prescribing Principles and Medication Errors
Good prescribing principles are critical strategies for minimizing medication errors that may contribute to adverse drug events or patient fatalities.
Medication administration and dosing are some of the most critical components of healthcare. Improper dosing or mistakes during the prescription process contributes to thousands of healthcare complications each year and billions of dollars in healthcare spending. While providers follow good prescribing principles to dole out the appropriate medication and reduce error rates, the dosing protocols and some failures in the healthcare system account for many errors in patient care.
Each year, healthcare providers in the United States prescribe over 6,000 prescription medications in addition to the never-ending over-the-counter medications available to patients and caretakers.
While side effects are a widely understood component of medication use and drug administration, medication errors contribute to over 7,000 deaths in the US annually. Beyond fatalities, many reported and unreported adverse drug reactions and complications exist.
The National Coordinating Council for Medication Error Reporting and Prevention (NCC MERP) states that a medication error is “any preventable event that may cause or lead to inappropriate medication use or patient harm while the medication is in the control of the healthcare professional, patient, or consumer. Such events may be related to professional practice, healthcare products, procedures, and systems, including prescribing; order communication; product labeling, packaging, and nomenclature; compounding; dispensing; distribution; administration; education; monitoring; and use.”
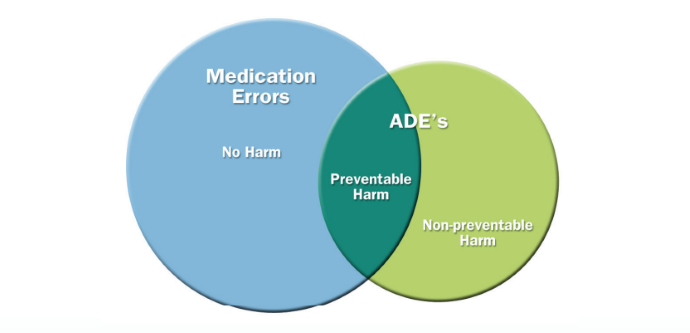
Beyond the broad definition of medication errors, the council also explains how medication errors are related to adverse drug events or reactions.
Medication errors that cause preventable harm are considered preventable adverse drug events (ADEs). However, there are also non-preventable ADEs, which are not considered medication errors and may include anaphylaxis due to an unknown allergy.
Below is a graphic from the NCC MERP illustrating the relationship between medication errors and ADEs.
Medication Error Statistics
According to the University of Oxford’s Center for Evidence-Based Medicine, adverse drug reactions cause roughly 2.5% of accidents and emergency department visits. Negative drug incidences account for 6.5% of hospital admissions, 15% of inpatient visits, and 25% of primary care visits.
A publication in StatPearls notes that medication-associated errors account for $40 billion each year in healthcare spending associated with morbidities and mortalities. The article revealed that the most common contributing factors to medication errors include the following:
- Failed drug communication orders
- Illegible handwriting
- Incorrect drug selection
- Drugs are mistaken for others with a similar name
- Packaging confusion
- Dosing errors with units or weight
- Human factors
There are multiple points in the prescribing process where errors could occur; however, StatPearls lists prescribing, ordering, documenting, transcribing, dispensing, medication administration, and monitoring as the most likely points of error.
Roughly 50% of medication errors arise during the order entry of the prescribing process. However, being an early phase of the prescribing process, this type of error may be identified and corrected before causing excessive harm. StatPearls notes that up to 70% of medication-ordering errors are identified by nurses and pharmacists when they double-check prescriptions.
Medication Error Causes
Understanding the point of error — when an error occurs — is critical; however, understanding the root cause is infinitely more valuable, as it can prevent future complications, improving patient safety. Some causes of medication error and the resulting patient outcomes are self-explanatory, while others indicate broader systemic issues in healthcare settings.
As discussed, incorrect prescribing or medication administration errors can contribute to ADEs. For example, a provider may prescribe or administer a medication at the wrong dose, strength, rate, timing, or duration.
Other factors that can cause ADEs are improper medication preparation or incorrect drug delivery. For instance, a provider may reconstitute a drug with the wrong formulation or give a medication through the incorrect route of administration, such as giving an intravenous injection subcutaneously.
Beyond the issues associated with improper prescribing, an inadequate medical history or medication reconciliation may lead a provider to prescribe a medication to which the patient has an allergy or contraindication.
The discrepancies above may happen at any point in the prescribing and administration process during hospital settings or outpatient care. Because of the various players in each process, it may be challenging to determine where the error began.
However, other errors can be directly attributed to a provider or sector of the healthcare industry. For example, pharmacists play a critical role in dispensing medications. A pharmacist's judgment or mechanical dispensing errors can contribute to various adverse drug events. For example, inadequate medication reconciliation, patient counseling, and incorrect dispensing can be common causes of medication errors.
While it is easy to push blame on pharmacists for making an error, a more holistic view implies a pervasive issue. Many clinical and retail pharmacists are burnt out. Exacerbated even further by the COVID-19 pandemic, short staffing and pharmaceutical burnout significantly contribute to medication errors.
Building on pharmacists’ burnout, exhaustion, and multiple duties across clinical practice is one of the most significant drivers of medication error. StatPearls notes that roughly 75% of all medication errors have been attributed to distractions.
Distractions or heavy clinical load may prevent providers from properly analyzing drug interactions or reviewing electronic health records, especially in acute care settings.
Additionally, case-specific scenarios may also cause prescription errors. For example, a patient’s age may impact medication sensitivity, making it a risk factor for medication errors. Pediatric and elderly populations are known to have increased sensitivity to medications. Not accounting for age and other patient-specific information can increase the risk of medication errors.
Finally, some medical interventions involve high-risk medications with more severe potential side effects. Patients on these medications must be monitored rigorously regardless of their care settings. When a patient is not adequately monitored — whether caused by patient or prescriber error — they are at an increased risk of adverse drug events.
Good Prescribing Practices
One of the best ways to minimize medication errors across all health services is to follow good prescribing guidelines. The University of Oxford proposes ten principles of good prescribing, including the following:
- Clarify the reason for prescribing.
- Consider the patient’s medication history.
- Evaluate the factors that may alter the medication’s or treatment's benefits and harms.
- Account for the patient's ideas, concerns, and expectations.
- Choose effective, safe, cost-effective medications depending on each patient.
- Follow national guidelines when appropriate.
- Write clear and legal prescriptions while documenting the data appropriately.
- Record and monitor beneficial and adverse outcomes of treatment.
- Record and explain prescribing decisions and reasoning.
- Prescribe using knowledge, skills, and experience.
The organization recommends that providers follow the mantra: “Choose wisely, inform, start low, and monitor.”
One of the first practices is to explain the cause of prescribing clearly. When possible, the provider must confirm an accurate diagnosis, clearly explaining the benefits of the medication to the patient. Often, a clear explanation and reasoning behind the functionality of the prescription can encourage patients to adhere to the treatment regimen better.
Another critical component of good prescribing is medication reconciliation, especially for patients taking several medications. Before prescribing, providers are expected to compare the potential prescription with the patient’s current medications, previous medications, allergies, and any adverse effects experienced on other drugs.
Other Ways to Minimize Medication Errors
The Academy of Managed Care Pharmacy (AMCP) focuses on how the system is flawed when a medication error occurs rather than blaming the individual clinician. While a prescriber’s negligence may contribute to medication errors, the AMCP suggests a closer look at the system in place to minimize or eliminate errors.
Medication errors should be reported to the Institute for Safe Medication Practices (ISMP) and the FDA reporting systems. Both organizations collect data and compile information to help mitigate the risk of future medication errors.
Multiple different factors have been used to minimize the risk of medication errors. Chief among the proposed plans is patient education.
Healthcare professionals are expected to provide the patient with in-depth information about the name of the medication, medication doses, frequency, and more. Although medication management involves clinicians, patients are responsible for ensuring that medications are taken appropriately. In pediatric cases, parents should take responsibility for managing medication safety.
The AMCP also suggests that prior authorization may be a helpful tool for minimizing prescribing errors, as it requires providers to review prescriptions and double-check their utility carefully.
One tool that may also improve medication safety is using electronic prescribing. While electronic prescribing is a widely used and relatively straightforward process, providers can easily view and compare a patient’s prescription, reducing the risk of faults.
Another tool for reducing the prevalence of medication errors is barcoding. According to the AMCP, “Medication barcoding is a tool that can help ensure that the right medication and the right dose are administered to the right patient. Today’s technology embeds increasing amounts of information within a scannable bar code on even the smallest packages.”
Barcoding has been adopted in many hospital settings to track and review medication dispensing, allowing hospitals to identify failures in their prescribing systems.
While medication errors can be unfavorable outcomes of the prescribing process and may lead to adverse events, fatality, loss of license, and more, clinicians and healthcare systems have many tools to identify and minimize errors and their public health impacts.







