
Getty Images/iStockphoto
The Complexities of Chronic Kidney Disease and Its Stages
Chronic kidney disease is a multifaceted, irreversible disorder that progresses in multiple stages.
Chronic kidney disease (CKD), referred to by nephrologists as the silent killer, is characterized by kidney damage that prevents waste filtering. According to the CDC, kidneys function as the filters for waste and toxins in the blood. Additionally, they manage blood pressure and assist in the creation of red blood cells.
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), a subset of the NIH, states, “the kidneys’ main job is to filter extra water and wastes out of your blood to make urine. To keep your body working properly, the kidneys balance the salts and minerals — such as calcium, phosphorus, sodium, and potassium — that circulate in the blood. Your kidneys also make hormones that help control blood pressure, make red blood cells, and keep your bones strong.”
Patients with CKD have lost some or all of that function depending on the stage of disease progression. The National Kidney Foundation (NKF) states that this declining function can lead to fatigue, trouble concentrating, eating, and sleeping, muscle pain, swollen feet, puffy eyes, dry skin, and increased frequency of urination, among other symptoms.
The NIDDK mentions that symptoms may be minor and even unnoticeable in the early stages of CKD. However, as the disease progresses, symptoms worsen and can impair quality of life. Advanced stage symptoms may also include chest pain, nausea, shortness of breath, vomiting, and weight loss.
Prevalence
Chronic kidney disease affects a relatively large portion of the population. The CDC declares that 1 in 7 people in the United States has CKD. It is one of the leading causes of death and impacts 37 million adults. Of people with CKD who are not on dialysis, approximately 40% do not know they have CKD, which may have implications for disease prognosis and treatment.
Diagnosis
CKD symptoms can be hard to notice in the beginning. However, if a physician suspects CKD or if a person has an increased risk of CKD, some tests can be done to determine the presence of CKD and its stage. The NIDDK identifies blood tests for determining the glomerular filtration rate (GFR) or urine tests to check for albumin as the primary diagnostic methods for CKD.
GFR tests the kidneys’ ability to filter waste, ranging from 0 to 120, with anything lower than 15 considered kidney failure.
The urine analysis measures the concentration of albumin, a protein found in the blood, to assess kidney function. The NIDDK states, “a healthy kidney doesn’t let albumin pass into the urine. A damaged kidney lets some albumin pass into the urine. The less albumin in your urine, the better.”
Additionally, kidney ultrasounds can be used to detect kidney damage.
Stages
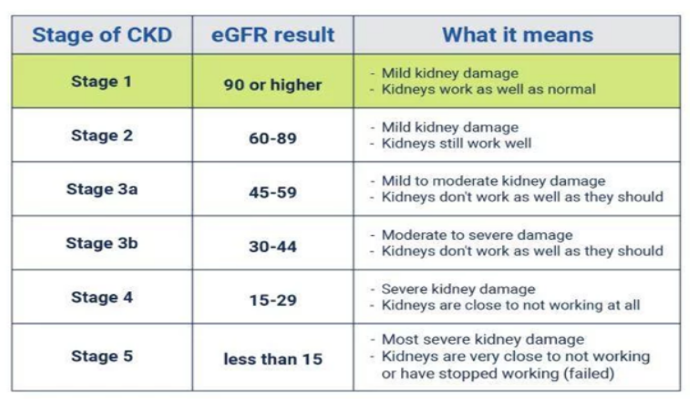
CKD is divided into five stages, with stage 3 split into two sections. As the stages progress, so does kidney damage. AKF shows that these stages directly correlate with the estimated GFR (eGFR). At stage 1, in which kidneys work well, patients have an eGFR of 90 or more. Conversely, stage 5, a complete lack of kidney function, is characterized by an eGFR of 15 or lower.
The other stages, 2, 3a, 3b, and 4, fall somewhere in between. Below is a graphic from the American Kidney Fund outlining each stage.
Risk Factors
Multiple factors can contribute to the development and progression of CKD, including comorbidities, race, age, genetic, and social aspects.
According to the NIDDK, the risk of kidney disease increases with age, and NKF identifies people over the age of 60 to be at higher risk for developing CKD. In part, this is due to natural aging.
“Many people don't realize that, as we age, we lose kidney function. Unfortunately, older Americans may not realize they are at increased risk until it is too late,” Beth Piraino, MD and NKF president, explains on the NKF “Aging and Kidney Disease” page.
The AKF states that Americans of African, Hispanic, Native, or Asian descent are at an increased risk of developing CKD.
The odds of getting CKD may also be associated with other preexisting conditions. Almost all sources cite diabetes and high blood pressure as being the leading cause of CKD. The CDC states that 75% of all new CKD diagnoses are caused by diabetes and hypertension.
Diabetes
The NIDDK explains that increased blood sugar in diabetes patients causes damage to blood vessels all over the body, including the kidneys. In the kidneys, the damage can cause a reduced ability to filter waste. The organization writes that approximately 33% of diabetic patients have CKD.
Hypertension
According to NKF, the relationship between CKD and hypertension is interchangeable. As stated on the NKF site, “if uncontrolled or poorly controlled, high blood pressure can be a leading cause of heart attacks, strokes, and chronic kidney disease. Also, chronic kidney disease can cause high blood pressure.”
Other Medical Risk Factors
Additional comorbidities that may increase the prospect of developing CKD include glomerulonephritis, polycystic kidney disease, kidney cancer, lupus nephritis, obesity, and heart disease.
Furthermore, a family history of chronic kidney disease increases the likelihood of developing the disorder.
Social Determinants of CKD
Despite medical risk factors being the most prominent contributing factors to CKD, multiple social factors can also contribute to CKD.
The NKF identifies multiple social determinants of CKD. Similar to the social determinants of health, these risk factors are environmental and social.
Food insecurity is a major social determinant of CKD. A healthy, low-sodium diet significantly reduces the risk of CKD. People struggling with food insecurity either lack access to food or adequate healthy food required to maintain blood sugar, minimize sodium intake, and sustain a healthy weight.
Housing insecurity and difficulty finding transportation can contribute to CKD risk by causing financial strain and limiting access to resources.
Environmental exposures also influence the probability of CKD diagnosis. Air and water quality, hazardous wastes, and community structures can impact physiological symptoms. As the ever-changing climate crisis worsens, so do the odds of CKD.
Prevention
Chronic kidney disease is a progressive and permanent disorder. Once the kidneys have been damaged, there is no way to undo them. However, multiple lifestyle aspects can contribute to slowing down or preventing the disease altogether.
As diabetes and hypertension are the most likely comorbidities to lead to CKD, managing and preventing these may mitigate the disease expansion. Managing diabetes and high blood pressure may include adjusting and adhering to a medication regimen.
Adopting a kidney-friendly diet may also diminish risks. The NIDDK states that a sodium intake of fewer than 2,300 milligrams with a diet of fresh fruits, fresh or frozen vegetables, whole grains, and low-fat or fat-free dairy products is ideal for preventing CKD.
Additionally, incorporating 30 minutes of exercise, developing healthy sleep habits, managing stress, and limiting smoking and alcohol intake may contribute to disease prevention.
Treatment and Management
Once diagnosed with kidney disease, patients must work with physicians to minimize or prevent progression.
The treatment for CKD is similar to its prevention as managing comorbidities, diet, and exercise are essential for CKD patients. The AKF also states that diuretics may be used to minimize kidney swelling by getting rid of salt and water.
In later stages or more severe CKD, dialysis may be used to assist the kidneys in filtering toxins. The last resort treatment for CKD is a kidney transplant.
Overall, CKD is an intricate chronic illness with multiple contributory factors. While not widely understood by the public, CKD has a high prevalence in the US. Unfortunately, CKD is not reversible, so prevention is essential. Maintaining a healthy diet and exercise routine and managing comorbidities are critical in disease management and prevention.






