
Getty Images
Preparing Patients for Stem Cell Transplants, Challenges
With a global average of 84,000 stem cell transplants occurring each year, providers are responsible for preparing patients for stem cell transplants and addressing the associated challenges.
In a 2022 article published in Haematologica, researchers note that approximately 84,000 stem cell transplants happen globally each year. Despite the lifesaving effects of a stem cell transplant, there are many associated challenges. The challenges of transplant begin before finding a donor and can carry on for years after the transplant. When preparing a patient for a stem cell transplant, understanding the potential challenges can help a provider address them and create a treatment plan based on the patient, donor, and reason for the transplant.
Stem Cell Transplants, Bone Marrow Transplants, and Hematopoietic Cell Transplant
Across hematology, providers may refer to stem cells, bone marrow, and hematopoietic cell transplants. Patients and less familiar providers may ask what the difference is. According to the American Society of Hematology (ASH), these terms are slight variations of the same concept. “All three terms refer to the same principle in which cells that can reconstitute the bone marrow are collected and infused,” states the ASH.
Depending on where the cells are extracted, providers may refer to the transplant in a specific form. This article uses stem cells, bone marrow, and hematopoietic cell transplants interchangeably.
Bone Marrow Transplant Basics
The Mayo Clinic defines a bone marrow transplant as “a procedure that infuses healthy blood-forming stem cells into your body to replace bone marrow that's not producing enough healthy blood cells. A bone marrow transplant is also called a stem cell transplant.”
There are two kinds of bone marrow transplants: autologous, which uses stem cells from the patient’s body, and allogeneic, which uses stem cells from a donor.
Reasons for Undergoing Transplant
The Mayo Clinic lists three main reasons for a bone marrow transplant. The first reason is for high-dose chemotherapy. Patients undergoing high-dose chemotherapy often have damaged bone marrow, and a transplant can replace it. Additionally, bone marrow transplants may replace bone marrow that does not interact well with new stem cells. Finally, a bone marrow transplant can introduce new stem cells to kill cancer cells directly.
Bone marrow transplants are beneficial for people with a range of diseases, including but not limited to acute leukemia, aplastic anemia, lymphoma, neuroblastoma, plasma cell disorders, and immune deficiencies.
Stem Cell Transplant Risk
Despite the benefits of a bone marrow transplant, the procedure can be complex and risky for the recipient and the donor. Risks and side effects may vary from minor, treatable complications to life-threatening complications.
Possible complications include graft-versus-host disease, graft failure, organ damage, infection, cataracts, infertility, new cancers, and death.
Graft-versus-host disease (GVHD) only occurs in allogeneic transplants. GVHD is comparable to organ rejection in traditional organ transplants. This happens when the patient’s body sees the donor’s stem cells as a pathogen or a foreign entity rather than a medication. The patient’s immune system may then attack the grafted stem cells.
GVHD is a common complication of allogeneic stem cell transplants, occurring in nearly all patients with an allogeneic transplant. GVHD can be acute or chronic. Acute GVHD presents in the first few months following transplant and can impact the skin, liver, or digestive tract. Chronic GVHD develops after those first few months with symptoms including joint or muscle pain, difficulty breathing, persistent cough, visual changes, dermatological changes, jaundice, dry mouth, nausea, vomiting, and diarrhea.
The Transplant Process
Preparing for a stem cell transplant is a complicated process requiring many steps. Providers conduct a host of tests to ensure that the patient can handle the difficulty of the transplant and minimize the risk of GVHD.
According to the Mayo Clinic, before a bone marrow transplant, the provider assesses the patient’s general health, which may include a series of tests or procedures. Once the patient is deemed eligible for the transplant, a central line is put in. It is used for the duration of the treatment to deliver the donor or autologous stem cells as well as medications and other biological products.
After testing, patients also undergo a process called conditioning — meant to “condition” the body in preparation for receiving a stem cell transplant. Conditioning typically involves at least one round of chemotherapy but may also involve additional rounds or radiation to destroy existing cancer cells and suppress the immune system. Immune system suppression may also reduce the risk of GVHD.
Conditioning side effects include nausea, vomiting, diarrhea, hair loss, infection, bleeding, infertility, anemia, fatigue, or organ complications.
For some patients, providers may choose reduced-intensity conditioning, equating to lower doses or different types of chemoradiation.
Finding a Match
For allogeneic transplants, the process also involves finding a match. According to Be the Match, a cheek swab is taken from donors to determine whether they would be a close bone marrow match for a specific patient. The cheek swab collects human leukocyte antigen (HLA), a better indicator of bone marrow match than blood type.
Be the Match notes that the immune system uses HLA markers to deem specific cells as belonging to the patient or foreign. The organization states, “many HLA markers make a person’s tissue type unique; however, matching certain markers is critical to a successful transplant.”
Willing donors can have their cheek swabbed and their data put into the Be the Match registry. Providers searching for a bone marrow match for their patients can look at this registry and identify suitable matches.
The standard check swab looks at six HLA markers. Luckily, providers typically find several donors who have a basic match to their patient using the registry. Then the donors are asked to do additional blood or check swab tests to determine the best match.
According to Be the Match, “About 8% of members who complete additional testing will go on to donate. If a member is asked to donate, that means they are the closest HLA match to the patient — the best donor.”
Unfortunately, the likelihood of finding a bone marrow match varies based on ethnicity. Be the Match states that the possibility of finding a match using its registry ranges from 29% to 79%.
The organization notes that the HLA markers used to determine whether a donor is a good match are usually inherited. Below is a graphic highlighting the likelihood of finding a match by ethnicity.
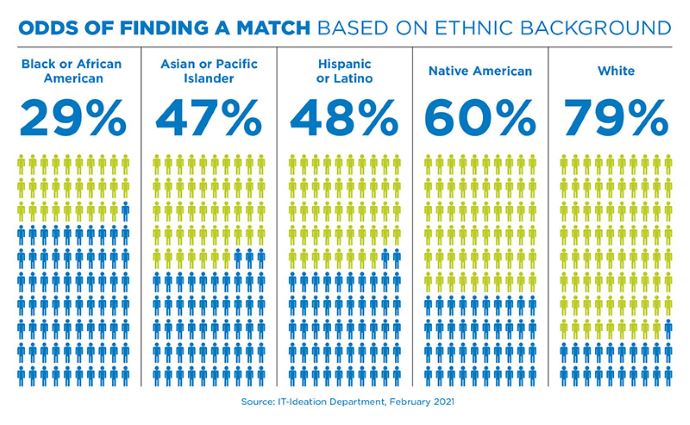
Ernesto Ayala, MD, told the Mayo Clinic, “The biggest challenge that we have to find donors to proceed with bone marrow transplantation is ethnicity. If I have a patient that belongs to an ethnic minority, then I will only find a donor in the registry about 20–25% of the time.”
Collecting Stem Cells for Transplant
To collect stem cells for autologous transplant, patients undergo apheresis, where blood is drawn and circulated into the machine to separate the blood components. Stem cells are then extracted and frozen for future transplant while the remaining blood is returned to the body. Before apheresis, patients receive growth factors to increase stem cell production and allow for easier collection.
Once a match is found for allogeneic transplants, stem cells are extracted from the blood or the bone marrow, depending on the patient and donor’s needs.
Additionally, the Mayo Clinic notes, “another type of allogeneic transplant uses stem cells from the blood of umbilical cords (cord blood transplant). Mothers can choose to donate umbilical cords after their babies' births. The blood from these cords is frozen and stored in a cord blood bank until needed for a bone marrow transplant.”
Post-Transplant Care
After conditioning, patients will receive stem cells through a central line. After the transplant, the body begins an engraftment procedure where the stem cells travel to the bone marrow and multiply, creating new cells. Patients will be monitored for several weeks after the transplant with regular blood tests to monitor the progress of engraftment. Providers may also consider transfusing red blood cells and platelets until the patient’s body begins making its own.
According to the Mayo Clinic, patients may be prescribed medications to reduce the risk of GVHD and other infections.
Other considerations following the transplant include diet and lifestyle factors. Many patients who have had a bone marrow transplant see a nutritionist to help them develop a diet that will mitigate excessive weight gain and minimize chemotherapy and radiation side effects.
Transplant Costs
According to a 2012 publication in Blood, the average cost of a single autologous stem cell transplant can vary from $36,000 to $88,000. For patients with an allogeneic procedure from an unrelated donor, prices can be as much as $200,000.
Researchers in Blood note that stem cell transplants “generated the most rapid increase in total hospital costs from 2004 to 2007 with a growth rate of 84.9% and $1.3 billion spent in 2007.”
The publication in Blood notes that many factors may contribute to these costs, including patient characteristics, transplant center, conditioning, graft type, length of hospital stay, and complications.







