
elenabs/istock via getty images
Navigating Male Reproductive Care in a Post-Roe World, Vasectomies
As patients, providers, and public health experts work to navigate male reproductive healthcare in a post-Roe world, addressing common misconceptions around vasectomies can help clinicians provide more comprehensive patient consultations.
Across the United States and the world, people with female reproductive anatomy shoulder most of the contraceptive burden as few male contraceptive methods are available. Aside from condoms and contraception currently being researched, vasectomies are the only form of male contraception.
In the current post-Roe landscape, more people with male reproductive organs are becoming interested in vasectomy procedures. Despite the newfound curiosity, many misconceptions about vasectomies are widespread. Understanding common misconceptions and being equipped with the facts allows clinicians to provide comprehensive consultations to patients seeking a vasectomy.
Vasectomy Rates in a Post-Roe World
The American Journal of Men’s Health notes that approximately 500,000 vasectomies are performed in the US each year; however, following the Supreme Court decision to overturn Roe v. Wade, healthcare facilities have seen a spike in interest in getting a vasectomy.
In an article published by the American Academy of Medical Colleges (AAMC), the organization revealed rising interest in vasectomies in the post-Roe landscape, noting that for many this form of contraception has become a political act as a result of the fears surrounding reproductive access.
According to the AAMC, before the overturning of Roe v. Wade, there was already a significant increase in the number of people interested in acquiring vasectomies. This increase marked a 2.5 times increase in vasectomy inquiries in 2022 compared to 2021.
In an interview with the University of Florida Health, Kevin Campbell, MD, assistant professor at the department of urology at the University of Florida College of Medicine, shared that “in June 2022, vasectomy rates nationally increased by 50%. At UF Health, we typically perform 40 vasectomies each month. In the first week of July, we had double the normal number of patients calling to make an appointment for a vasectomy.”
What Is a Vasectomy?
Vasectomies are a form of birth control meant for those with male reproductive organs to prevent sperm release. Vasectomies block the vas deferens, preventing sperm from traveling from the testicles to the urethra. According to Hopkins Medicine, the patient still makes sperm; however, without the ability to be released, the sperm dies and is absorbed by the body.
Hopkins Medicine notes, “A man who has had a vasectomy still makes semen and is able to ejaculate. But the semen doesn't contain sperm. The testosterone level and all other male sex traits stay the same. For most men, the ability to have an erection is unchanged.”
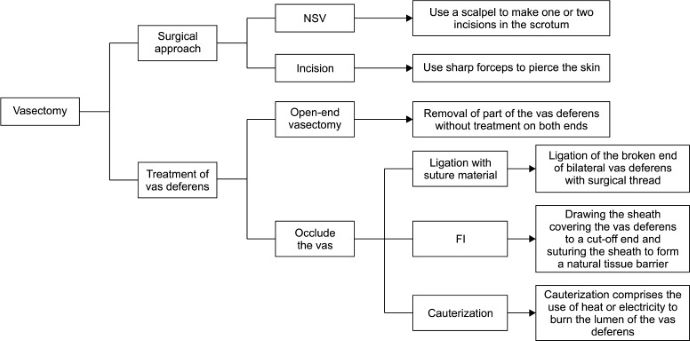
There are different methods of vasectomy; however, the two most common are incision and non-scalpel vasectomies (NSV). NSVs do not use an incision; instead, forceps create a small hole in the skin.
Below is a flowchart graphic from the World Journal of Men’s Health outlining the varying types of vasectomies.
Side Effects
While generally, vasectomies are safe, like any surgery, they are not without risks, including sperm granuloma, infection, epididymitis, orchitis, procedure failure, long-term pain, short-term bleeding, swelling, and bruising. Other common complications may include hematoma formation, infection, sterilization failure, post-operative pain, and chronic pain syndrome.
Infection
The rate of infection and hematoma development after a vasectomy can vary dramatically, with some sources noting that incidence is 3–4% and others citing incidence rates as high as 29%. According to the World Journal of Men’s Health, the surgical technique significantly impacts infection risk, with NSVs having a lower incidence of hematoma and infection. Many patients can have a vasectomy without experiencing post-surgical infections or hematoma, assuming proper protocols are enforced.
Providers may consider prophylactic antibiotics — although not commonly used for this procedure — for patients more susceptible to infection.
Post-Vasectomy Pain Syndrome
Another potential side effect is post-vasectomy pain syndrome (PVPS), characterized by scrotal pain that lasts for a minimum of three months after surgery without epididymitis or other causes.
While there is little understanding of the pathophysiology of this condition, researchers in the World Journal of Men’s Health note, “Retrospective case series and prospective observational and follow-up studies suggest that chronic pain follows vasectomy in 1–15% of men, but only about 1–2% of men noted that it affected their quality of life. The average time until the onset of PVPS is 7–24 months. Demographic characteristics (age, socioeconomic status, and ethnicity) and surgical techniques have not been shown to be associated with the occurrence of PVPS.”
Sperm Granulomas
Sperm granulomas are another common occurrence following vasectomies, usually appearing within three weeks of surgery at the vasectomy site, the epididymis, or the testicular rectum. This condition is a “granulomatous lesion that constitutes a foreign-body giant cell reaction to the extravasated sperm.”
Sterilization Failure or Insufficient Sterility
Although vasectomies are seen as a very effective contraceptive method — with the American Journal of Men’s Health noting that vasectomies are a 99.9% effective permanent contraceptive method — many providers warn against sterilization failure and insufficient sterility. According to the Cleveland Clinic, in approximately 1 out of every 10,000 patients who get a vasectomy, sterility may not be achieved as sperm can cross the severed ends of the vas deferens.
In addition to sterilization failure, Johns Hopkins Medicine recommends avoiding intercourse following a vasectomy. The organization notes, “A man can often start having sex again soon after vasectomy. But another birth control method should be used. This is because some sperm may stay in the vas deferens for some time after surgery. Other birth control should be used until the surgeon tests the semen to be sure there are no sperm left. This is often about three months after surgery.”
Misconceptions
As previously mentioned, many patients have misconceptions about the risks and benefits associated with vasectomies. Comprehensive care includes consulting patients and clarifying any misconceptions before proceeding. For some patient populations, education may clear up misconceptions deterring patients from acquiring a vasectomy.
Prostate Cancer
One common misconception is that vasectomies can cause prostate cancer. This notion is rooted in early data on vasectomies, suggesting that it may be associated with higher prostate cancer rates. However, other researchers also noted that patients who have had a vasectomy tend to have better prostate cancer survival rates. This statistic has left many patients confused about vasectomies and their risks.
However, many researchers attribute this phenomenon to the fact that individuals willing to undergo vasectomy are more likely to get regular prostate cancer screenings. Investigators in the World Journal of Men’s Health note a weak correlation with no biological justification for the link between vasectomy and prostate cancer.
Sexual Dysfunction
Another possible side effect of vasectomy is sexual dysfunction; however, this is an unlikely side effect, and several studies have shown the opposite relationship. Many studies suggest vasectomies can improve erectile function, sexual satisfaction, and sexual confidence.
Reversibility
Despite common misconceptions, vasectomies are not always reversible as the procedure was developed to be permanent. While some people can reverse the procedure, the University of Florida notes that only about 6% of patients will attempt to reverse the procedure as it can be an extensive process.
According to Planned Parenthood, vasectomy reversal can be tricky with risks such as scrotal bleeding, infection, and chronic pain. Additionally, vasectomy reversal can cost up to $15,000, although they are only successful about 85% of the time.
Additionally, Planned Parenthood carefully notes that reversal is not synonymous with fertility. Only about 55% of patients who have a vasectomy reversal can impregnate their partners. With this in mind, those looking to conceive in the future without reproductive assistance may decide against vasectomy.
Researchers in the World Journal of Men’s Health concluded, “Numerous reports have confirmed that vasectomy is a safe, reliable, and low-complication method for male birth control.” Despite the benefits, vasectomies' complications and side effects must still be discussed. Providers are obligated to clarify and share this information to ensure adequate, comprehensive male reproductive healthcare.






