How Do Social Isolation and Loneliness Impact Healthcare Outcomes?
As the epidemic of social isolation and loneliness increases globally, especially in the US, understanding the healthcare impacts of these conditions is critical.
In 2023, the United States Department of Health and Human Services (HHS) published an advisory from the US Surgeon General on the national epidemic of loneliness and isolation. The report highlighted the multiple risks associated with increased levels of loneliness.
“Social connection — the structure, function, and quality of our relationships with others — is a critical and underappreciated contributor to individual and population health, community safety, resilience, and prosperity,” noted the Surgeon General in the advisory.
To emphasize the critical impact of loneliness on health, his report noted that social isolation, or lacking social connections, can increase the risk of early death at an intensity that is comparable to smoking 15 cigarettes daily.
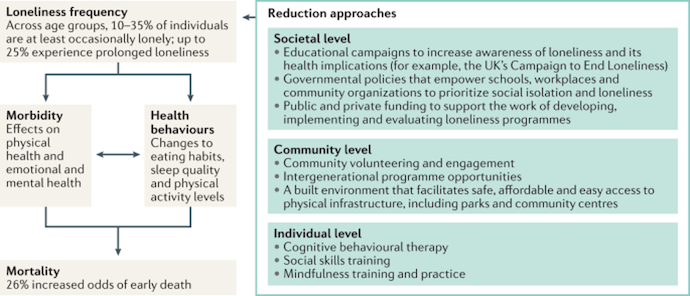
The CDC notes that marginalized communities, including older adults, immigrants, and members of the LGBTQ+ community, are more likely to experience loneliness and social isolation. Although there is no precise explanation, some individuals theorize that loneliness and social isolation are more prevalent among these populations due to stigma, discrimination, and social barriers.
“Although it’s hard to measure social isolation and loneliness precisely, there is strong evidence that many adults aged 50 and older are socially isolated or lonely in ways that put their health at risk,” the CDC notes.
Loneliness v. Social Isolation
An article published in Nature Reviews Disease Primers notes that loneliness and social isolation or a lack of social connection are not synonymous; however, the subjective feeling of loneliness can arise from the objective status of social isolation.
The HHS defines social connection as a combination of interactions, relationships, roles, and a feeling of connection among individuals, communities, and society. The following three traits can characterize social connection:
- Structure, which refers to the number or variety of relationships and frequency of interactions
- Function, which is how much a person can rely on certain connections
- Quality, which considers how satisfied an individual is with their connections
Beyond describing the three characteristics of social connection, the US Attorney General’s advisory noted that social connection is a dynamic continuum that ebbs and flows on a sliding scale. Additionally, he revealed that adequate social connection does not necessarily equate to good health but may be associated with lower disease risks in some cases.
The CDC defines loneliness as feeling alone regardless of social contact, while social isolation is actually having reduced social connections.
Unlike depression and anxiety screening tests with distinct scores, there are minimal measurements of loneliness. Most healthcare professionals assess loneliness using questions like “How often do you feel lonely,” and other questions related to loneliness.
Rates of Social Isolation
According to the CDC, approximately one-third of adults 45 or older in the US have felt lonely. Moreover, a quarter of US adults 65 and older are considered socially isolated.
In addition to the standard high rates of loneliness and social isolation experienced by elderly and senior populations, the COVID-19 pandemic and the subsequent quarantines have caused increased rates of loneliness across all age groups.
Over the past few years, Americans have reported lower levels of social connection, with reduced social participation on individual and community levels.
According to the 2023 loneliness advisory from the US Surgeon General, trust amongst US citizens is declining. Beyond increasing levels of distrust nationwide, the report pointed out many jarring changes in social networks and participation.
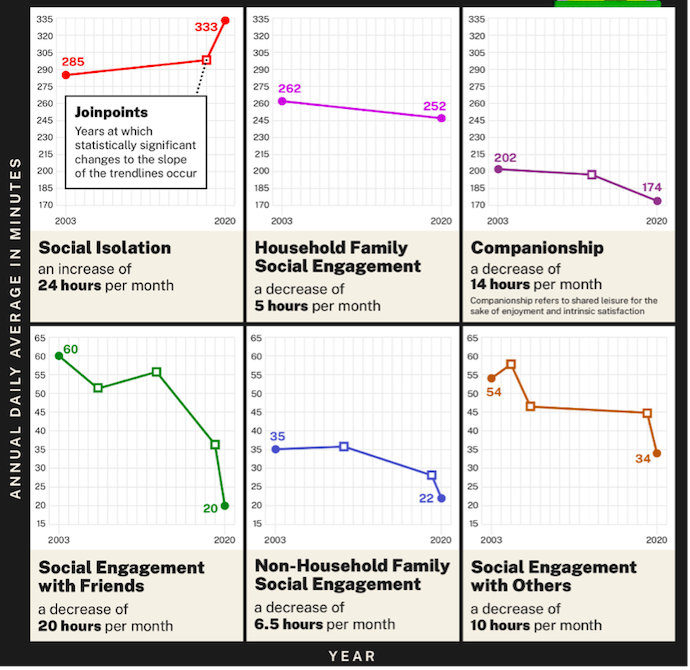
For example, the average time spent alone, which could be used to depict social isolation, increased from 285 minutes daily in 2003 to 333 minutes daily in 2020. Although the report does not provide measurements for subsequent years, the onset of the COVID-19 pandemic and quarantine protocols likely increased this number dramatically.
Additionally, social participation rates, represented by the amount of time spent engaging with friends in person, declined from 60 minutes per day in 2003 to 20 minutes per day in 2020.
More trends in social connection are depicted in the graphic below.
“While profoundly disruptive in so many ways, the COVID-19 pandemic offers an opportunity to reflect more deeply on the state of social connection in our lives and in society. As we emerge from this era, rebuilding social connection and community offers us a promising and hopeful way forward,” noted the advisory.
Risk Factors
Multiple factors may increase the risk of social isolation and loneliness. The CDC considers the following as risk factors:
- A low income
- Psychiatric or depressive disorders
- Being a part of a marginalized or discriminated group
- Living in a rural area or other barriers to resources
- Stress associated with limited access to resources
- Chronic conditions
- Long-term disabilities
- Living alone
- Experiencing violence or abuse
- Going through significant life changes, including divorce, job loss, or loss of a loved one
Health Impacts of Social Isolation
The CDC notes that social isolation has been linked to all-cause premature mortality at significant rates comparable to the risks of premature mortality from smoking, obesity, and physical inactivity.
Focusing on individual health outcomes, the HHS advisory revealed that social isolation and loneliness correlated with higher mortality rates. Aggregated data from nearly 150 studies found that social connection improves survival outcomes, increasing the probability by 50%. Conversely, social isolation is linked to higher mortality risks compared to other lifestyle, traditional clinical, and environmental risk factors.
One theory is that social isolation can contribute to multiple other health conditions, increasing mortality risk.
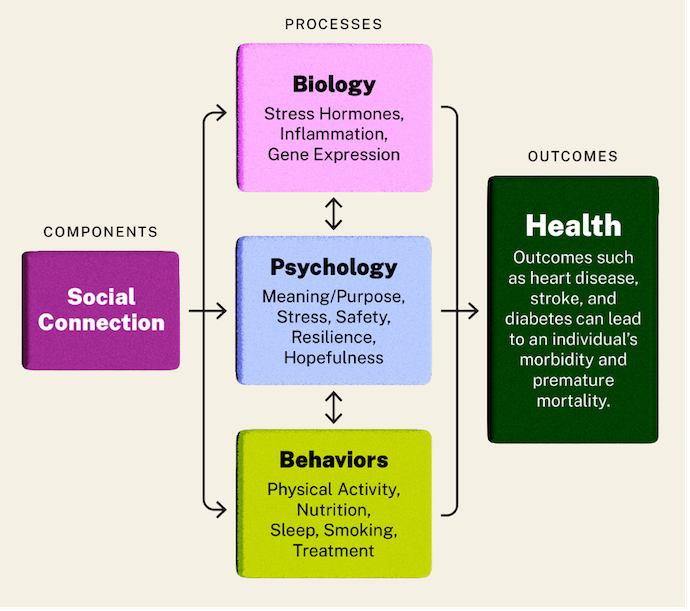
The report notes three primary ways social connections impact health: biology, psychology, and behaviors.
Cardiovascular Health and Hypertension
Some studies have linked social isolation with an increased risk of cardiovascular disease, including heart disease and stroke. Poor social relationships — characterized by social isolation, poor social support, and loneliness — are associated with a 29% increased risk of heart disease and a 32% risk of stroke. In addition to an increased probability, these adverse events are more likely to occur early in life.
Among heart failure patients, those who reported being more lonely were at greater risk for adverse events, including hospitalization, emergency department visits, and outpatient visits. More specifically, inadequate social connection levels increased the probability of hospital readmission by over 50%.
Social isolation was also linked to elevated blood pressure or hypertension, which is a contributing factor to heart disease.
Diabetes
Looking at other chronic conditions, the Surgeon General noted that social isolation is associated with an increased risk of type 2 diabetes and related disease complications. Unlike type 1 diabetes, which is generally not addressed with lifestyle changes, type 2 diabetes is often traced back to lifestyle factors such as diet and exercise.
In addition to an increased risk of diabetes and complications associated with social isolation, social connection is linked to improved outcomes across patients with diabetes. Researchers theorize that social networks and support systems promote improved diabetes management by allowing patients to engage in better personal care habits, including medication adherence, physical activity, balancing nutrition, and more.
Analysis of the National Health and Nutrition Examination Survey revealed that elderly diabetic individuals with a more extensive support system, including six or more close social connections, had a reduced risk of all-cause mortality.
Infectious Disease
Shockingly, socially isolated individuals are also more susceptible to infectious diseases. The advisory from the US Surgeon General notes that these individuals have weaker immune systems, making them more vulnerable to disease.
Individuals who take on six or more social roles are four times less likely to develop colds than those who take on fewer social roles, irrespective of previous exposure and existing antibody count.
Neurological Conditions
Cognitive function is also significantly impacted by social isolation. Adults who reported feeling lonely were at an increased risk for dementia and cognitive impairment, with probabilities rising by as much as 50% regardless of other contributing factors.
Lonely or socially isolated individuals also experienced cognitive decline at a 20% faster rate than those who are well-connected.
Psychological Diseases
Moreover, depression, anxiety, suicidality, and self-harm risks are significantly higher among socially isolated or lonely individuals. Adults who report feeling lonely are more than twice as likely to be diagnosed with depression and similarly likely to have an anxiety diagnosis.
In his advisory, the US Surgeon General cites a 2010 study called The Interpersonal Theory of Suicide, which notes, “Social isolation is arguably the strongest and most reliable predictor of suicidal ideation, attempts, and lethal suicidal behavior among samples varying in age, nationality, and clinical severity.”
According to the Nature Reviews article, poor behavioral and emotional control and inadequate sleep quality have been linked to loneliness.
Addressing Social Isolation
There have been multiple recommendations for managing social isolation and connection as a determinant of health. While the US Surgeon General highlights a multitude of options, some of them include the following:
- Acknowledging social connections as a healthcare priority
- Incorporate social connection into medical education
- Integrate social connection into patient care
- Make social connection a research priority
Evidence pointing to loneliness or social connection as a social determinant of health suggests that more research and funding should be allocated toward addressing the loneliness epidemic in the US.







