
AlfaOlga/istock via Getty Images
How Antirejection Drugs Can Promote Successful Transplants
Antirejection drugs are complex and significantly promote a successful transplant before and after the procedure.
The United Network for Organ Sharing (UNOS) states that, as of July 2022, there have been 24,414 organ transplants this year in the United States alone. Considering the limitations on the number of organs available for transplant and the potentially life-altering outcomes, clinicians work relentlessly to ensure successful transplants. Antirejection drugs play a significant role in promoting successful organ transplants. Despite the proven success of these medications, their astronomical costs adversely impact medication adherence.
The Basics
Antirejection medications, also known as immunosuppressive medications, are essential for organ recipients following a transplant.
The University of California San Diego Health Center (UCSD Health) states that antirejection medications work by blocking the immune system. This can prevent it from attacking the new organ; unfortunately, it also prevents the immune system from attacking viruses, bacteria, and other infections.
“Most of the immunosuppressants are powerful drugs and, hence, have side effects. For some of them, levels in the blood are to be monitored frequently. Too little of the drug will put you at risk for rejection, while too much might mean side effects. So, it takes your caregivers some time to achieve the right balance of immunosuppression,” wrote Pradeep Kadambi, MD, for the National Kidney Foundation (NKF).
Types of Antirejection Medications
According to Kadambi, antirejection medications belong to one of two categories: induction and maintenance agents.
“Think of a real estate mortgage — the down payment serves as the induction agent, and the monthly payments serve as maintenance agents. If the down payment is good enough, you can reduce the monthly payments substantially, and the concept is similar for immunosuppression,” stated Kadambi in his article for NKF.
Induction agents are used during the transplant and are particularly powerful, while maintenance agents are used after the transplant to help maintain patients’ health.
Dosage
A proper dosage of immunosuppressive drugs is necessary for transplant recipients, as a dosage that is too low can lead to insufficient suppression of the immune system. Conversely, an excessive dosage can completely wipe out a patient’s immune system rendering them unable to fight infection.
Duration of Use
Since the risk of rejection is highest right after surgery, the highest dose of antirejection drugs is prescribed at that time. Medication dosages typically stay consistent for the first six months after a transplant. Assuming the patient is recovering well, the six-month mark is the point at which medications are reduced.
According to the University of Michigan Medical Center, “kidney and pancreas transplant patients will need to take some combination of medications for the life of their transplanted organ. The types and amounts of medications may change over time, but all patients will need an ongoing medication regimen.”
Alongside Antirejection Drugs
Many clinicians know that antirejection medications alone are insufficient for a successful transplant. Kadambi says, “the success of transplantation depends on many factors. You need be adherent to your medications, exercise, and adopt a healthy diet and lifestyle. Other important issues include getting appropriate tests for cancer screening, always wearing sunblock, and getting vaccinated every year for flu and every other year for pneumonia,” in the NKF article.
Additional medications to manage blood sugar, pressure, or other bodily functions may be prescribed alongside the anti-rejection medications typically prescribed for transplant recipients.
Induction
Before a transplant, many patients at an exceptionally high risk of rejection undergo induction therapies. According to the University of Michigan Medical Center, “Induction therapy helps the recipient “tolerate” the new organ. Thymoglobulin is the most commonly used medication for induction therapy, although there are several others, including Simulect.”
Maintenance
Under the maintenance agents are calcineurin inhibitors, antiproliferative agents, mTOR inhibitors, and steroids.
Depending on the patient, their condition, and other clinical factors, these drugs can be combined in multiple ways. While that is the case, the NKF states that the most common combination includes tacrolimus, mycophenolate mofetil, and prednisone.
While mTOR inhibitors and steroid medications are typically only taken once daily, calcineurin and antiproliferative inhibitors are taken twice daily. The NKF urges patients to adhere strictly to medication times as it yields the best results.
Although these drugs present many benefits to transplant patients, they are not without drawbacks. Generally, the most common side effects of antirejection medications are stomach pains.
Calcineurin Inhibitors
Calcineurin inhibitors include tacrolimus and cyclosporine. Calcineurin inhibitors block messages that lead to rejection. These medications are taken twice daily, with each dose taken 12 hours apart and often needed for a lifetime.
Patients will receive either tacrolimus or cyclosporine but should never be taking both at the same time. Tacrolimus is given as a 0.5, 1, or 5 mg capsule. Potential side effects include kidney toxicity, high blood pressure, diabetes, diarrhea, hair loss, and neurotoxicity.
Cyclosporine is given as a 25 or 100 mg capsule and may cause nephrotoxicity, neurotoxicity, high blood pressure, excessive hair growth, and gout.
Patients taking these drugs should inform their providers of all their medications to avoid interactions. Additionally, the University of Michigan Medical Center advises that patients taking this medication avoid consuming grapefruit as it alters drug levels in the blood.
Antiproliferative Agents and mTOR Inhibitors
Antiproliferative agents may include mycophenolate mofetil, mycophenolate sodium, and azathioprine. Antiproliferative agents stop the replication of immune cells, reducing the number of cells able to attack the new organ.
Based on the brand, mycophenolate is also prescribed twice daily, varying from 180 to 500 mg. These medications can cause low blood cell and platelet count, diarrhea, cramps, nausea, and vomiting.
The most common mTOR inhibitor used as an antirejection mediation is sirolimus.
Steroids
Finally, the most common steroid is prednisone. Immediately following transplant, prednisone is prescribed twice each day in one of the following dosages: 1, 2.5, 5, 10, 20, or 50 mg. Once a patient is discharged after a transplant, this dosage is decreased and tapered. Side effects of prednisone include the following:
- facial, hand, or feet swelling
- appetite and weight changes
- stomach problems
- acne
- mood swings
- water retention
- diabetes
- high blood pressure or cholesterol
- insomnia
- muscle fatigue
It is strongly encouraged that this medication is taken alongside food.
According to Kaiser Permanente, steroids “reduce inflammation and prevent rejection of the organ. For the first few days after your transplant, you'll likely have a high dose. Then the dosage is slowly reduced to the lowest dose that helps prevent rejection. Taking steroid medicine for just a few days may cause short-term side effects. These include high blood pressure, weight gain, sleep problems, and anxiety. High doses can sometimes cause more severe side effects, such as extreme agitation, paranoia, psychosis, and hallucinations.”
An Overview of Side Effects
Below is a graphic from the University of Michigan Medical Center summarizing the side effects of common antirejection medications.
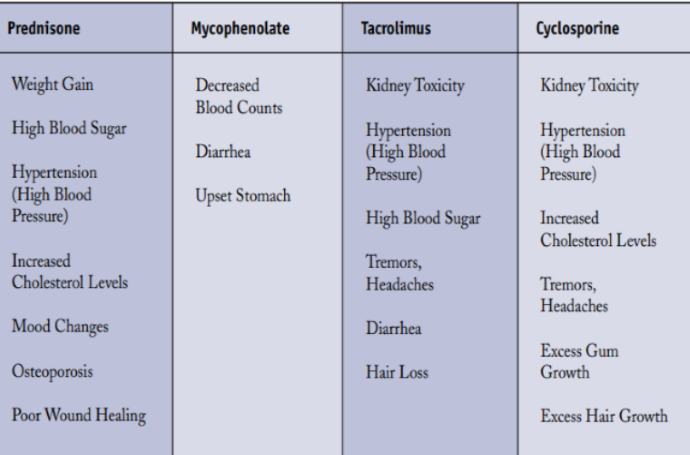
Despite the listed side effects, not everyone will experience all or any of the side effects of these medications.
Cost of Medications
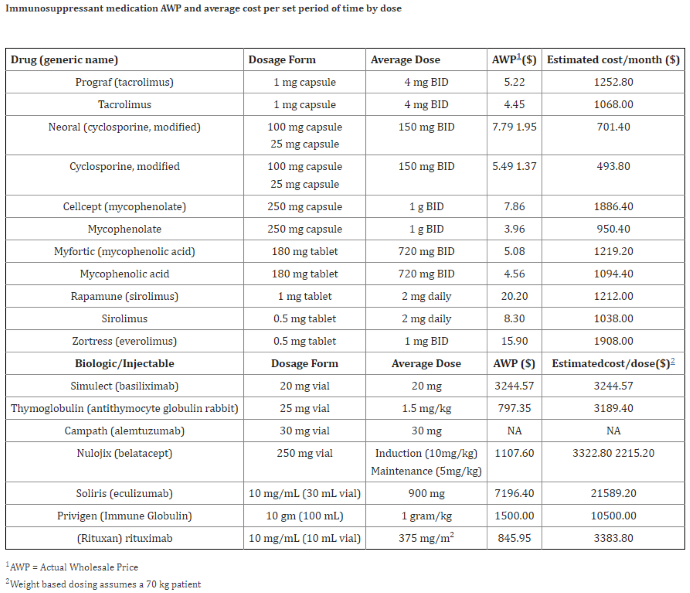
According to a 2016 publication in Current Transplant Reports, the average transplant cost at the time ranged from $260,000 to $1.2 million.
Researchers in the publication state that “long-term oral maintenance immunosuppression and other prescription medications can cost patients upward of $2,500.00 per month depending on various factors including the number of prescription medications, insurance coverage, with the average annual cost of medications in the United States reported between $10,000 and $14,000 per patient.”
While the costs are reduced after one year, there is still a financial burden on patients and the healthcare system. UVA Health highlights multiple organizations that assist in funding transplants, including the National Foundation for Transplants.
Below is a graphic from Current Transplant Reports outlining the average costs of common antirejection drugs.
There are many proven benefits associated with antirejection drugs. These immunosuppressive medications serve many roles beyond their position in transplant care. Providers who work directly with patients receiving these medications should make themselves aware of the potential side effects and the proper dosing regimen.
Additionally, patients struggling with the costs of antirejection medicines should inform their healthcare provider and seek assistance from one of the available programs. Medication adherence is essential to a successful transplant. Stakeholders, including patients, payers, providers, hospitals, and more, should remain invested in the affordable and accessible distribution of these medications to those who need them.







