
Getty Images
Geroscience: targeting aging mechanisms for preventing chronic disease
Geroscience is an emerging field focusing on understanding and addressing aging mechanisms to avoid age-related chronic diseases.
Perhaps one of the only definite predictions in healthcare is that patients will age. With age comes a host of complications and age-related conditions that require attention from patients, providers, and the entire healthcare system. But what if aging could be slowed down? What if the underlying mechanisms of aging could be targeted to prevent the host of conditions associated with this biological process? That is precisely the question geroscience researchers are hoping to answer.
Aging and Geroscience
According to a 2023 article in Nature Communications, behavioral changes, public health efforts, and medical advancements have expanded lifespans far beyond what could have been imagined centuries ago; however, as life expectancy increases, the incidence of chronic disease and multiple morbidities has also increased.
“Relative to life expectancy, these can result in a prolonged period of decreased health that can last over a decade. The increases in life expectancy that have outpaced increases in healthspan in some countries are characterized by increased disability, diminished quality of life, and high healthcare costs,” noted the researchers in the article.
A 2023 article in the Journal of the American Geriatric Society notes that scientists’ understanding of aging and its underlying processes has advanced significantly over the past few decades. From discovering mutations in genes that impact lifespan to new insights into the evolution of aging, researchers have begun to get a clearer picture of aging, its implications on health, and its mechanisms.
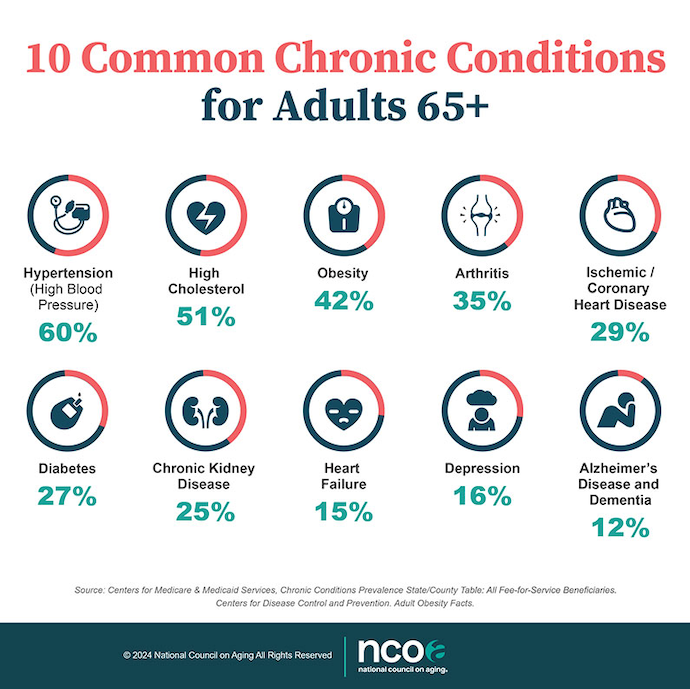
According to the journal, aging is one of the most significant risk factors for chronic diseases such as diabetes, cardiovascular disease, cancer, and dementia. The National Council on Aging lists the 10 most common chronic conditions for adults 65 and older.
As the understanding of aging advanced, scientists discovered methods to manipulate biological aging rates, including behavioral changes, genetic modifications, and medications.
Targeting aging to prevent chronic disease is an emerging field of research known as "geroprotective medicine" or "geroscience." While the field is still developing, several therapeutic interventions show promise in slowing down the aging process and reducing the risk of chronic diseases.
The NIH notes that geroscience focuses on understanding the genetic, molecular, and cellular components of aging and why those factors make it a major risk factor for chronic disease.
In This is Growing Old, a podcast from the Alliance for Aging Research, Felipe Sierra, PhD, noted that geroscience is based on the understanding that aging is the major risk factor for nearly all chronic diseases and addressing aging altogether instead of the individual pathophysiologies of chronic diseases.
Researchers in the Journal of the American Geriatric Society wrote, “This multidisciplinary field is grounded in the Geroscience Hypothesis, which states that strategies designed to modify biological drivers of aging will not only slow the progression of biological aging but will also prevent or delay the onset of multiple chronic diseases.”
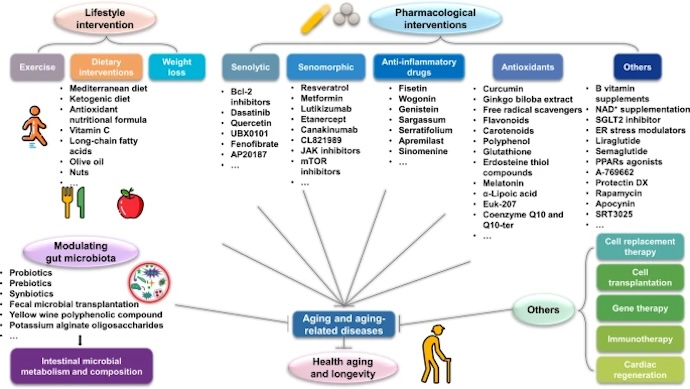
According to a Nature Portfolio collection, geroprotective interventions are therapeutic tools that tackle the biological causes of aging. The result is preventing age-related decline and age-related diseases. Early research into biological aging and therapeutic interventions for disease prevention focused on dietary restriction and manipulating caloric intake to prevent aging.
Caloric Restriction
Limiting calorie intake without malnutrition has been shown to extend lifespan and improve health in various organisms. Caloric restriction mimetics, such as drugs or compounds that mimic the effects of calorie restriction, are currently being investigated for their potential to delay aging and age-related diseases.
According to a 2022 article from the National Institute on Aging, nearly a century ago, Cornell researchers found that animal models fed lower-calorie diets that contained the appropriate nutrient levels lived longer than those fed higher-calorie diets. This discovery gave way to the theory that caloric restriction could extend healthy life years.
Since the primary discovery, the NIA launched the CALERIE study in 2012, which showed that moderate calorie restriction could diminish risk factors for age-related diseases.
Pharmacological Interventions
However, more recent research has assessed how pharmacological approaches may impact lifespan. Certain drugs and compounds, such as rapamycin, metformin, and senolytics, have shown potential in extending lifespan and improving healthspan in animal models. Clinical trials are underway to evaluate their safety and efficacy in humans.
While researchers continue exploring pharmacotherapeutics to address aging and expand lifespans, the research has been predominantly in animal models.
“There’s a lot of promise. There’s dozens and dozens of potential, what we call, gerial protectors, molecules that can protect you from the ravages of aging. They have been tested in many animal models, but we’re just starting to test them in humans and only in the context of diseases, not for aging itself; that will take a long time and a lot of money to do,” Sierra said in the Alliance for Aging Research’s podcast.
Senotherapeutics
Laura Niedernhofer at the University of Minnesota is one researcher focusing on the emerging geroscience field. As part of her research, she studies senescent cells, aging cells that can no longer multiply but remain in the body without dying off.
According to the University, 3–10% of cells in older adults are senescent. Although these cells play a critical role in tumor suppression and wound healing, research has shown that they may also trigger the immune system, causing inflammation and making individuals more susceptible to age-related diseases.
Niedernhofer is working alongside Paul Robbins and the Mayo Clinic to research a class of drugs called senotherapeutics. These include senolytic drugs to clear senescent drugs from the body and senomorphic drugs to modify senescent cells.
An article in Signal Transduction and Targeted Therapy outlines other areas of exploration in geroscience beyond lifestyle changes, pharmaceutical interventions, and senotherapeutics.
Challenges and Opportunities in Geroscience
There are multiple challenges associated with developing geroscience trials.
Researchers in Nature Communications note that government agencies such as the FDA and the European Medicines Agency (EMA) define indications for treatments as diseases or manifestations of disease, which means that they typically don’t classify aging as a treatable indication.
Based on these concerns, the researchers believe a primary goal for geroscience is defining approvable indications.
According to the Journal of the American Geriatric Society, geroscience is currently working on accomplishing five goals:
- Translating animal models into humans: The journal notes that, while animal trials have provided some insight into aging, human aging is unique and may have more complicated factors.
- Recruiting midlife and older adult participants: Since social and behavioral factors contributing to aging begin early in life, understanding geroscience cannot start when patients are older. Additionally, the journal notes that preventing damage in midlife adults may be easier than trying to reverse damage in older adults.
- Developing tools to measure the pace of aging: The ability to measure the pace of aging can provide insights into the effects of geroprotective interventions sooner, as clinical endpoints may take a long time to assess.
- Assessing baseline aging pace: As an extension of the previous goal, understanding baseline aging rates is critical for evaluating whether interventions impact that pace.
- Implementing the benefits of geroscience in populations that would benefit: The journal notes that marginalized communities tend to have the fastest aging paces, die the youngest, and are the least likely to participate in clinical trials; however, widespread impacts of geroscience require that all populations are included in research and treatment.







