
traffic_analyzer/DigitalVision V
Clinical Pharmacists Are a Major Contributor to Quality Patient Care
As the popularity of clinical pharmacists continues to rise, understanding their role, history, and benefits shows that they significantly contribute to quality patient care.
In recent years — especially considering the COVID-19 pandemic — the public has become increasingly aware of pharmacists’ role in healthcare. Despite the current prevalence of clinical pharmacists and their position on care teams, the clinical pharmacy industry was not always as widespread as it is today. Between the 1960s and the 1990s, the pharmaceutical industry experienced a massive overhaul as pharmacists began to take on a new direct patient care role.
What Is Clinical Pharmacy?
To understand the rise of clinical pharmacy, it is essential to understand what clinical pharmacy is. Northeastern University states that there are five key kinds of pharmacists, including community, long-term care, consultant, industry, and clinical pharmacists.
The American College of Clinical Pharmacy (ACCP) states that a clinical pharmacy is “an area of pharmacy concerned with the science and practice of rational medication use.” This position is a very collaborative role that is most often found in hospitals or community health centers.
Roles of a Clinical Pharmacist
According to the ACCP, a clinical pharmacist works directly with healthcare professionals such as physicians to optimize the medications prescribed for the best patient outcomes. Clinical pharmacists are notably different from other pharmacists as they have regular direct patient contact. Most clinical pharmacists are in medical centers, clinics, and other healthcare facilities.
The ACCP states that most clinical pharmacists have patient care privileges granted by physicians or the facility where they work, assuming that the pharmacists have completed the necessary education and experience.
The roles of clinical pharmacists are vast, including the following:
- assessing patient’s health problems and medication lists
- evaluating medication efficacy
- monitoring patient progress
- educating the patient on proper medication usage and side effects
- collaborate with the patient’s healthcare team
One of the primary goals of clinical pharmacy is comprehensive medication management (CMM).
“The definition of CMM is the standard of care that ensures each patient's medications (prescription, non-prescription, supplements, or herbals) are individually assessed to determine if appropriate for the patient, effective for the condition, safe for use with concurrent comorbidities and therapies, and that the patient is able to take them,” states an article in the Revista Médica Clínica Las Condes.
Clinical pharmacists must review all the patient’s prescribed and unprescribed medications and supplements to ensure that there will be no drug interactions that may cause adverse side effects or unfavorable patient outcomes.
Standards of Practice
While clinical pharmacists are expected to follow the traditional process of care that all pharmacists follow, as seen in the figure below, they also take on some additional roles.
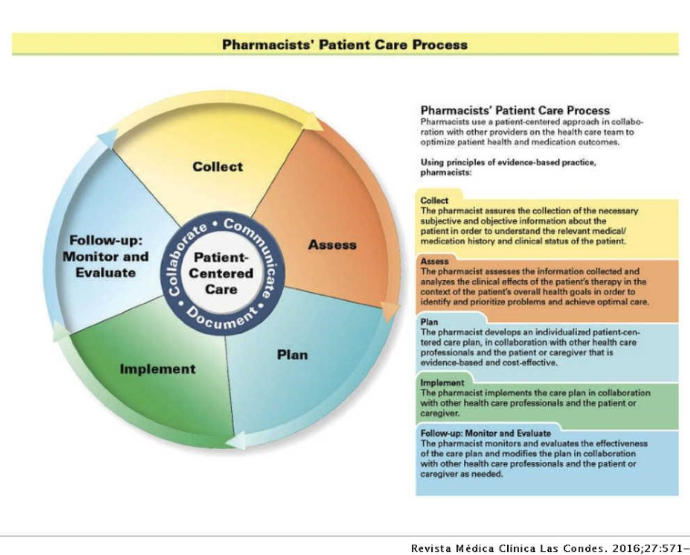
Besides the aforementioned patient care process, clinical pharmacists may manage more complex treatment regimens and may be required to take more detailed clinical notes. Because of their direct patient contact, they may also be more involved in the patient billing process.
Clinical Pharmacy Education
The educational requirements for a clinical pharmacist are slightly more extensive than for a regular pharmacist.
History of Clinical Pharmacy Education
To understand the educational requirements for a clinical pharmacist, it is essential to look back at how education evolved. According to the IOSR Journal of Pharmacy and Biological Science, in the late 1920s, the University of Iowa Hospital was the first healthcare facility to allow pharmacists to participate in patient rounds. Looking back, this was the very beginning of clinical pharmacies.
Over 20 years later, the University of Southern California launched the first doctor of pharmacy (PharmD) course. A publication in Drugs Aging states that the PharmD degree was first recommended in 1950 after a long-winded conversation about pharmacists and the requirements for their formal education.
By 1955, only two universities, the University of California San Francisco and the University of Southern California, had implemented these degrees. It wasn’t until the late 1960s that other universities began implementing their own programs.
“Finally, in 1992, the AACP House of Delegates voted to approve the PharmD degree as the only professional degree in pharmacy, doing away with the Bachelor of Science in Pharmacy. The American Council on Pharmaceutical Education (ACPE) is the body that sets educational standards and accredits colleges of pharmacy. In 1997, the ACPE decreed that they would no longer accredit Bachelor of Science programs effective in 2000 and all colleges of pharmacy had to convert to the PharmD as the sole professional degree,” stated Barry L. Carter, PharmD, in the article in Drugs Aging.
In addition to the degree changes made to alter the education of pharmacists, there were multiple advancements made in postgraduate education. Postgraduate residencies and clinical pharmacy training were concurrently expanding alongside schooling. According to the publication, in 1962, the first hospital pharmacy residence was established to help postgraduate pharmacists develop leadership skills and other traditional traits. Down the line, additional, more patient-focused residencies were established as well.
Current Pharmacy Education
Clinical pharmacy education has come a long way since its start in the late 1920s. In the United States, clinical pharmacists undergo six years of schooling before obtaining a PharmD degree. While a bachelor’s is not required for this degree, many do obtain one.
Following graduation from a PharmD school, pharmacists can opt for additional education via a postgraduate residency. These residencies are meant for pharmacists who intend to have a direct patient care role. An additional residency year can be done for those hoping to focus on more specialized care settings. Other educational opportunities may include fellowships that allow clinical pharmacists to specialize in pharmacy for nearly any medical specialty.
Benefits of Clinical Pharmacy
As seen throughout the COVID-19 pandemic, clinical pharmacies and pharmacists play a critical role in the health and well-being of patients. They assist the care team and educate patients to yield the best possible outcomes.
Examples of Benefits
In his publication in Drugs Aging, Carter notes that many studies, including the CAPTION trial, found that clinical pharmacists and clinical pharmacy practices have significantly improved patient outcomes. Collaboration between pharmacists and physicians to treat, educate, and advise patients has improved the management of chronic conditions.
The publication states that the CAPTION trial was a multicenter prospective clinical trial across 15 states and analyzed the impacts of no, brief, or sustained physician–pharmacist collaborative interventions on managing blood pressure.
According to the article, by the nine-month mark, the subjects who had an intervention had a blood pressure that was an average of 6.1 mm Hg lower than the subjects without an intervention. This was observed across all races and ethnic groups. “This study found that the pharmacist intervention could be implemented in a large number of diverse primary care offices and that the intervention was effective in under-represented minorities and patients from low socioeconomic groups,” concluded the publication.
Looking Ahead
As the popularity of clinical pharmacists has grown, many anticipate that clinical pharmacists will continue to be valuable members of the patient care team. Physicians and other healthcare professionals managing patients with chronic conditions may consider consulting clinical pharmacists.
As stated in Revista Médica Clínica Las Condes, “while the clinical pharmacy programs are in various stages of development globally, the need for specialists with a broad focus on medications and their optimal use is universal. The American College of Clinical Pharmacists has supported these training programs and provided education to individuals and groups. Their publications are used for the preparation and maintenance of board certification by pharmacists worldwide. This outreach is expected to continue, as more partners are engaged and more pharmacists and their multi-professional teams recognize the opportunities for clinical pharmacists to improve patient care.”







