
Getty Images/iStockphoto
Applications of Psilocybin in Mental Health Disorder Treatments
A recent revolution in psychedelics has caused researchers to explore the applications of psilocybin in mental health disorder treatments.
Over the past few years, researchers have explored psychedelics, including lysergic acid diethylamide (LSD), ketamine, 3,4-methylenedioxymethamphetamine (MDMA), and more for treating mental health disorders. Among the many psychedelics being explored for clinical use, psilocybin has become a significant part of psychedelic research.
According to a 2019 article published in Cureus, the first isolation and synthesis of psilocybin was done in 1958 by Albert Hoffman. In 1967, psilocybin and other classic hallucinogens were classified as Schedule I substances by the United Nations Convention on Drugs.
The United States Drug Enforcement Administration (DEA) notes that psilocybin, sometimes called magic mushrooms or shrooms, is a hallucinogen extracted from psilocybe mushrooms.
Although the drug has been used recreationally to cause hallucinogenic effects, clinical researchers and scientists have explored the potential mental health benefits of the medication. While psilocybin is a controlled substance classified as a Schedule I drug, researchers postulate that the medication may have a low abuse potential as symptoms of dependence and withdrawal have not been reported.
The first regulatory approval to resume psychedelic research after they became controlled substances was granted to Hopkins researchers by the US Food and Drug Administration in 2000.
Mechanism of Action
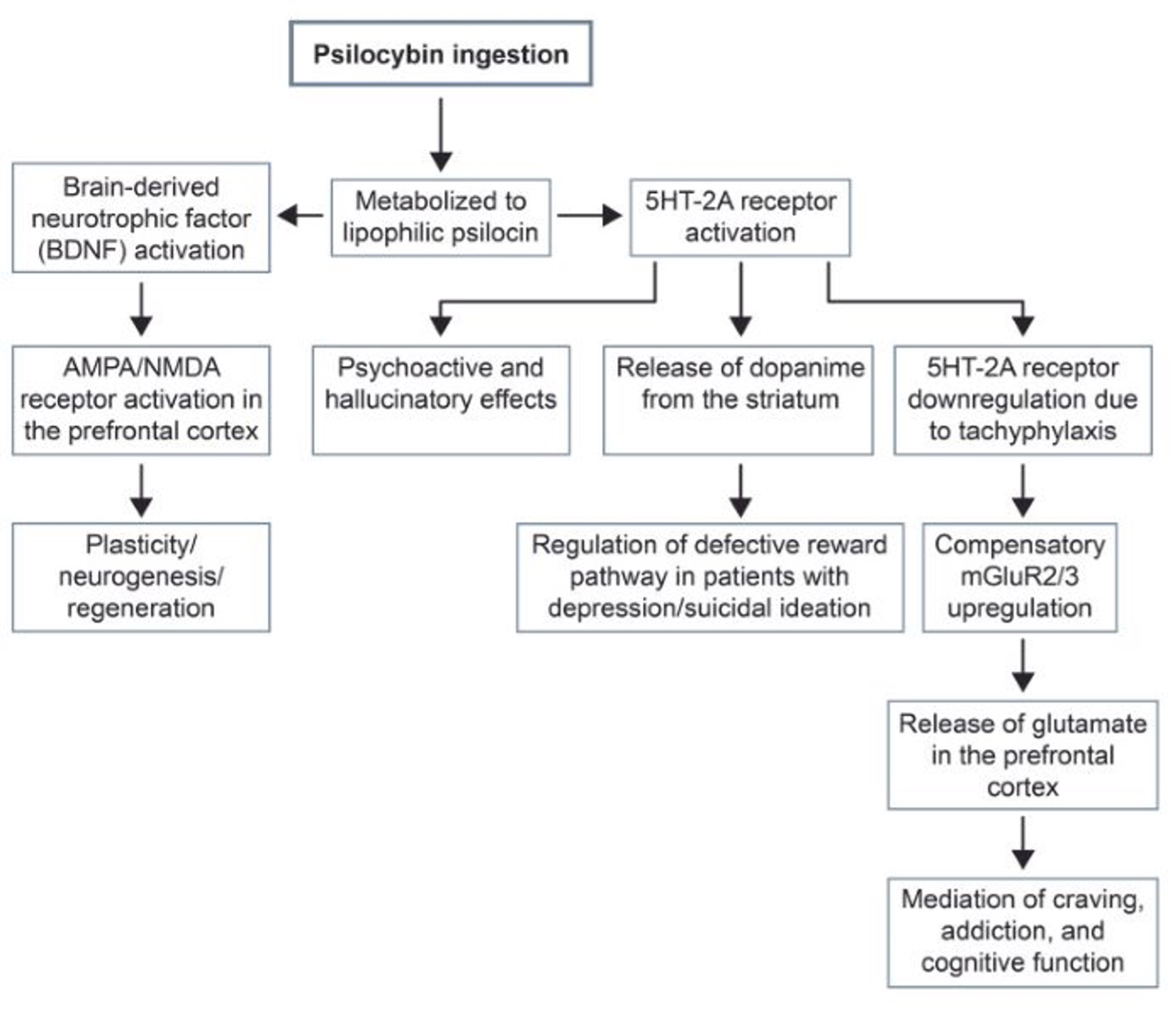
Researchers in Cureus note that psilocybin and other classic psychedelics are similar to tryptophan and act as serotonin receptor agonists. The National Institutes of Health (NIH) notes that psychedelic drugs can promote neuroplasticity by binding to and activating 5HT2A receptors.
Serotonin receptors are located in multiple areas of the brain, including the cerebral cortex and thalamus. Activating these receptors in the thalamus can lead to sensory changes and hallucinations.
Once ingested or administered, psilocybin is converted into psilocin, a more lipophilic version of the drug that can pass the blood–brain barrier.
Below is a graphic from Cureus that outlines the different mechanisms of action of psilocybin.
Additionally, the drug has a favorable pharmacokinetic profile, with peak effects beginning within an hour and a half. Compared to traditional treatments, including antidepressants, psilocybin has a much faster action time.
In addition, the side effects or adverse events linked to psilocybin are much milder than some other treatments. Side effects include transient hypertension, tachycardia, minor headaches, and short-term psychosis.
A 2022 systematic review published on the potential therapeutic effects of psilocybin notes that it can have psychological or somatic impacts. Some psychological effects of psilocybin include affective activation, hypnagogia, dreams, introspective thoughts, and mystical experiences. Sometimes these psychological symptoms are referred to as a “bad trip.”
The somatic effects include the following:
- Mydriasis
- Altered heart rate or blood pressure
- Nausea
- Changes in reflex dysmetria
- Tremors
Psilocybin has been explored for each of the following conditions, with a varying amount of evidence:
- Cancer-related depression
- Cancer-related anxiety
- Treatment-resistant depression
- Alcohol use disorder
- Tobacco addiction
- Obsessive–compulsive disorder
- Cluster headaches and migraines
- Demoralization with AIDS diagnosis
Substance Use Disorders
One of the main clinical uses of psilocybin is substance use disorder treatment. Clinical research between the 1950s and 1970s pointed toward a significant benefit of psilocybin and other psychedelic drugs for addiction treatment. Another advantage of the drug is that it only requires 2–3 treatments to be effective for substance use disorder.
Psilocybin therapy has been used to address nicotine addiction and prompt smoking cessation. A 2014 pilot study led by Matthew W. Johnson, published in the Journal of Psychopharmacology, analyzed the effects of moderate and high dose psilocybin on smoking cessation.
The clinical trial recruited psychologically healthy volunteers who identified as nicotine-dependant smokers. On the target smoking cessation date, patients were given a 20 mg/70 kg dose of psilocybin. At 7 and 13 weeks, patients were given higher doses of psilocybin (30 mg/70 kg).
The study found that roughly 80% of participants ceased smoking based on an evaluation at their six-month follow-up. Compared to other behavioral or pharmacological treatment methods, which have an efficacy of under 35%, the use of psilocybin was significantly more effective.
The effects of psilocybin were much more pronounced when compared to FDA-approved treatments for smoking cessation. For example, only 24.9% of patients on bupropion for nicotine addiction abstained at six months.
Alcohol use disorder is another use case for psilocybin. The drug has been proven to reduce heavy drinking days significantly.
A 2022 clinical trial published in JAMA Psychiatry recruited patients between 25 and 65 with alcohol dependence. The 12 trial participants were observed over 32 weeks. Each patient received two doses of either psilocybin or diphenhydramine at four and eight weeks. Patients also were enrolled for 12 psychotherapy sessions distributed before, after, and between sessions.
At the close of the study, patients receiving psilocybin had 9.7% heavy drinking days, while those taking the control had 23.6% heavy drinking days. Conclusions from this study point to the benefits of psilocybin for alcohol use disorder.
Depression
Beyond uses for substance abuse, psilocybin has also been effective in managing major depressive disorder (MDD).
Standard treatment for patients with MDD includes psychotherapy and antidepressants, often selective serotonin reuptake inhibitors (SSRIs).
While these drugs are effective for some patients, SSRIs can take a long time to work and may be linked to adverse side effects. Researchers estimate that between 30% and 50% of patients have treatment-resistant depression (TRD) that does not respond to SSRIs.
A 2020 study published in JAMA Psychiatry recruited 27 patients between 21 and 75 years old with moderate-to-severe unipolar depression, with a score greater than 17 on the GRID-Hamilton Depression Rating Scale (GRID-HAMD).
All patients were given two doses of psilocybin; however, one group was treated immediately while the other group had delayed treatment, with the first session starting at eight weeks. Only 24 participants completed the study and the one-year follow-up.
The treatment was considered adequate if the patient had a greater than 50% reduction in GRID-HAMD score. Approximately 75% of patients had a treatment response, and 58% achieved remission.
Additional studies have been conducted on using psilocybin for mental illness, including moderate-to-severe major depressive disorder. A 2021 Phase 2 double-blind, randomized controlled trial led by Robin Carhart-Harris found that psilocybin led to a 57% remission rate at 6 weeks, compared to a 28% remission rate for patients treated with escitalopram.
Another study published in the New England Journal of Medicine revealed that a single dose of psilocybin can reduce Montgomery–Åsberg Depression Rating Scale (MADRS) score in patients with TRD.
Obsessive–Compulsive Disorder
Psilocybin has also been explored in treating obsessive–compulsive disorder (OCD). A 2022 case study published in Heliyon noted that psilocybin could significantly reduce OCD symptoms in a patient with refractive OCD.
The 33-year-old male had a history of MDD, Tourette syndrome, and panic disorder alongside his primary diagnosis of OCD. The patient’s Yale–Brown Obsessive–Compulsive Scale score declined from 24 to between 0 and 2.
Additionally, an ongoing double-blind, placebo-controlled clinical trial conducted by researchers at Yale Medicine is analyzing the efficacy of psilocybin in OCD treatment.
Anxiety
Psychedelic treatments, including psilocybin mushrooms, have been explored to manage end-of-life mood disorders and anxiety or depression linked to life-threatening cancer.
Throughout the years, multiple studies have been done on psilocybin to address cancer-related anxiety or depression. For example, a 2016 study by Roland Griffiths at Johns Hopkins University confirmed that high-dose psilocybin treatment yielded a 78% response rate and a 65% remission rate after a six-month follow-up.
Despite the well-known therapeutic benefits of psilocybin, there is very little information or guidance for healthcare providers interested in psilocybin-assisted psychotherapy.
While the FDA has recently issued some guidance on researching psychedelics to promote a better understanding of their effects, pharmacology, and psychopharmacology, additional research and regulatory acceptance of psilocybin is necessary to understand its therapeutic benefits fully.





