
Getty Images
US Maternal Mortality, Maternal Health Disparities, Worsened Since 2019
Maternal mortality and maternal health disparities are only getting worse in the US, even as the nation acknowledges a need for data-driven and community-based solutions.
Maternal mortality, plus maternal health disparities, continue to get worse, as the Centers for Disease Control and Prevention (CDC) reports the worst figures for maternal mortality in the past few years.
This comes as the US has the unenviable ranking as the worst in the developed world for maternal health equity.
Drawing on the definition from the World Health Organization, CDC stated that a maternal death is “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and the site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.”
Maternal deaths in the United States were higher in 2021 than they were in years previous, reaching 1,205 deaths. That shakes out to a maternal mortality rate of 32.9 deaths per 100,000 live births.
Those figures fare poorly when compared to the years before. 2020 saw 861 maternal deaths and a maternal mortality rate of 23.8, while 2019 saw 754 maternal deaths with a rate of 20.1.
These numbers account for birthing people of all races and ethnicities. When broken down by demographics, the CDC report showed that the maternal health equity problem in the US is also getting worse. Maternal mortality rose for non-White groups at a faster rate than for White people.
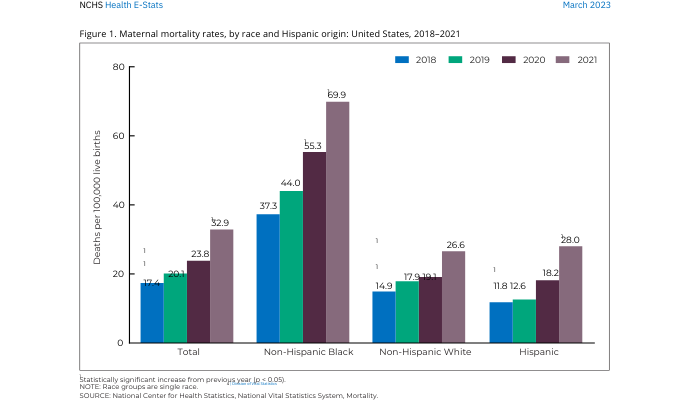
The maternal mortality rate for non-Hispanic Black birthing people was 69.9 deaths per 100,000 live births, or 2.6 times the rate for non-Hispanic White birthing people. That compares to a maternal mortality rate of 55.3 deaths per 100,000 live births in 2020 among Black birthing people, the CDC said.
That year-over-year increase is steeper than for White or Hispanic people. For White people, the maternal mortality rate rose from 19.1 deaths per 100,000 live births to 26.6. For Hispanic people, that increase was 18.2 to 28 deaths per 100,000 live births.
Those unequal increases demonstrate that, despite calls to the contrary, the US hasn’t ameliorated its Black maternal health disparities problem. Of course, a centuries-old problem isn’t going to be fixed within a few years. This latest CDC data shows that the nation needs to stay the course on addressing maternal health equity through data-driven and community-based solutions.
There were also age-based disparities, the CDC continued. In 2021, the maternal mortality rate for individuals over age 40 was 138.5 deaths per 100,000 live births. That compares to rates of 20.4 and 31.3 per 100,000 live births among those under age 25 and those between 25 and 39, respectively.
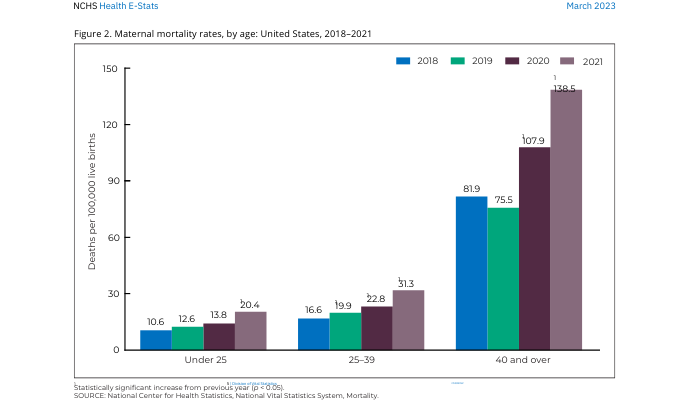
Those numbers shake out to a maternal mortality rate that is 6.8 times higher for those over age 40 compared to those under age 25.
Higher maternal mortality rates among older birthing people are unsurprising, considering the higher risk pregnancy later in life carries.
But the US Census Bureau has reported that younger birthing people are largely deferring pregnancy until later in life, as birth rates increase among birthing people in their 30s and 40s. As this trend continues, the healthcare industry should investigate strategies to help mitigate adverse outcomes among those giving birth later in their reproductive age.






