
Adene Sanchez/E+ via Getty Image
Patient education tips for GLP-1, weight loss drug treatment
Obesity treatment is not a one-and-done process. Patients taking a GLP-1 need to be supported by multidisciplinary care teams that practice strong patient education strategies.
GLP-1 medications have taken the healthcare industry by storm because of their unprecedented ability to address the chronic illness of obesity in a non-invasive way.
As more GLP-1 prescriptions are written to manage not just diabetes and cardiovascular disease but also obesity, a key question emerges: What is the role of patient engagement and chronic disease management when prescribing these drugs?
Indeed, GLP-1s are incredibly effective at triggering weight loss on their own. If a patient were to just take the medication without any kind of lifestyle or behavior change, they could expect to lose between 15% and 20% of their body weight, depending on the specific GLP-1 they're taking.
"But because what we know about obesity care is evidence-based, we don't typically approach it that way. We don't just say, 'Hey, take the drugs, see you in a year,'" said Enrica Basilico, MD, a weight loss specialist with Providence Swedish in Seattle, in an interview.
Obesity is a chronic illness, just like diabetes and cardiovascular disease, Basilico and experts like her agree. Like other chronic diseases, obesity needs a holistic approach to care that certainly can include medical intervention, such as GLP-1s, but it also needs strong patient engagement and activation.
How do GLP-1s work?
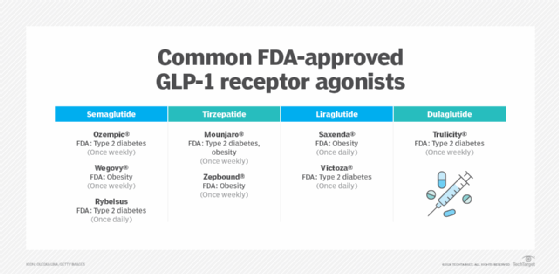
GLP-1 receptor agonists (RAs) work by mimicking a hormone that helps regulate blood glucose levels and insulin. When blood sugar levels rise after eating, the medication triggers the body to produce more insulin, which in turn can lower blood sugar levels. For that reason, many of these medications are FDA-approved and indicated for diabetes treatment.
GLP-1s can also promote feelings of fullness, prompting FDA to approve some drugs as weight loss agents. In some cases, clinicians have also prescribed GLP-1 drugs off-label for weight loss. However, Medicare and private payers have yet to determine whether they will cover the medications for weight loss, primarily citing concerns about cost and potentially high utilization rates.
Depending upon the type of GLP-1 taken, patients can expect to lose up to 20% of their total body weight. However, experts clarify that not all patients react to GLP-1s the same. Weight loss is usually distributed on a bell curve.
There are also side effects to taking GLP-1s, most of which are related to gastrointestinal issues. GLP-1 side effects can include the following:
- Nausea.
- Constipation.
- Gas.
- Bloating.
- Heartburn.
- Diarrhea.
- Intestinal cramping.
- Muscle loss.
- Weakness.
Despite the side effects and murky insurance coverage, GLP-1s are becoming more common weight loss interventions.
May 2024 data from KFF showed that 6% of adults currently take any GLP-1 drug, with 12% saying they have taken the medications at any point in time. Of adults taking or who have previously taken a GLP-1, 62% said they took it for diabetes or heart disease, while four in 10 said they took it to treat obesity.
Understanding obesity as a chronic, relapsing illness
GLP-1s fold into the treatment conversation for obesity because the cultural discourse around obesity is changing. Increasingly, the medical community and the general public understand obesity to be a chronic, relapsing illness, as opposed to an overall moral failure. This means it has become more culturally acceptable to prescribe medical interventions to treat obesity.
Obesity is often defined by certain body mass index (BMI) metrics, but more generally, it is defined as bodily dysregulation, according to Lydia Alexander, MD, the president of the Obesity Medicine Association.
"Obesity is the dysregulation of an entire body process, which is weight, causing something that should not happen," Alexander said in an interview. "It's a malfunction, basically, of our body's ability to compute energy balance."
Individuals with obesity receive body signals telling them that they are hungrier, prompting them to find and consume more food to increase energy balance, Alexander added. This can happen for a variety of reasons and manifests differently in different people.
"Thinking of it that way, we would want to treat the root cause, and medications are one aspect of that because we want to improve the body signaling around hunger and energy balance," she explained.
GLP-1 medications fall neatly into the four pillars of obesity care management, Alexander and Basilico both said.
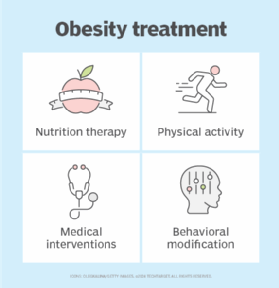
In addition to GLP-1 medications, interventions like bariatric surgery fall under the medicinal pillar.
Although medications alone can help reduce the number on the scale, this four-level approach to obesity care management is integral to long-term success.
"We've got the four pillars we rely on, and if you think of them as legs of a chair, every time you take one of them away, things don't work as well," Basilico explained. "All of these things go together, and our goal is not only to make people smaller but also to make people healthier and stronger, which is so powerful."
As more people explore the use of GLP-1 medicines -- KFF said about a third of adults had heard a lot about the drugs -- it will be integral for providers to practice holistic patient engagement and chronic disease management with their patients.
Starting GLP-1 use with shared decision-making
Like many medicines and treatments for chronic illnesses, the use of a GLP-1 is a decision that patients should make with the guidance of their providers. To that end, shared decision-making has to be part of the equation.
Obesity care providers start by taking a full weight history with patients, checking for relevant comorbidities and then discussing treatment options.
"And then, we discuss whether or not we're going to use a medical intervention," Basilico said, noting that some patients don't want to do a medical intervention. "We do informed consent, and we talk about the risks and the benefits of medications and the risks and the benefits of surgery so that people really understand what they are choosing between."
Basilico said she focuses on a few important aspects of the shared decision-making conversation with GLP-1s. Notably, these medications are extremely expensive, insurance coverage is variable and the U.S. is currently experiencing a GLP-1 drug shortage, all of which can complicate prescription access.
At each step in the shared decision-making process, clinicians need to identify a motivation for the patient to lose weight, according to Barbara Eichorst, MS, RD, CDCES, vice president of health care programs at the American Diabetes Association.
"Every person with diabetes is different, so we focus on problem-solving," she explained in an interview. "We always focus on what's most important to them and why they are taking this GLP-1. What do they want to achieve? We set up very realistic expectations, and then we help a person with diabetes to get where they want to get."
Eichorst primarily works with patients taking GLP-1s for diabetes management, not obesity care. So although weight loss might be the vehicle, it's not usually the destination; better diabetes management is. Knowing those personalized health goals will not only improve patient activation but can also help clinicians better tailor their treatments to individual patients.
Holistic care management
Although much of the current cultural discourse about GLP-1s is related to how the medications are used to manage weight, the fact of the matter is most patients (the KFF survey said around six in 10) are taking them to manage diabetes and heart disease.
Indeed, GLP-1 medications do stimulate the body to produce more insulin, effectively treating diabetes. But many patients with diabetes also take GLP-1 agonists to support weight loss, as weight loss itself can improve diabetes outcomes.
For that reason, much of the care management strategies employed when prescribing GLP-1 medications borrow from evidence-based obesity care management and diabetes care management.
"We know from the Diabetes Prevention Program that yes, if we improve weight without medication, if they're able to improve it by 5% to 7%, even that smaller amount of weight does improve people's different chronic conditions," Alexander explained. "We know that entails what is called intensive lifestyle intervention. We have to employ lifestyle measures and have them occur in a medical setting with team-based care to have lasting impact."
Alexander said that care management can be done in person or via telehealth, depending on patient preferences, the resources available and the reimbursement mechanisms at play. The important part is having a multidisciplinary care team featuring registered dieticians, health coaches, pharmacists, nurses and other licensed providers.
Clinicians and other specialized members of the care team can help guide patients in fitness and nutrition tracking, as well as weight tracking to monitor patient progress. According to Basilico, the effect GLP-1 drugs have on patients' appetites means there needs to be added emphasis on nutrition.
This is usually not a patient's first rodeo with nutrition counseling, Basilico emphasized. But because GLP-1s reduce a patient's appetite, there needs to be more counseling on the nutritional value of the foods the patients do eat, plus unwinding of maladaptive behaviors developed through various dieting attempts.
"We all know certain foods are healthier," Basilico said. "Well, how do we get them in our body? There's a lot of coaching and education about how we make our lives today work and eat foods that are healthier."
While it's important to have a comprehensive care team in place, Eichorst stressed the importance of making sure they're the right care team. The weight loss industry has been extremely commercialized, and there are a lot of snake oil salesmen out there.
Patients taking a medical intervention like a GLP-1 will want to surround themselves with credentialed providers who are certified to manage patients taking GLP-1s, she indicated.
What's the role of remote care providers?
Remote care providers have also entered the GLP-1 chat.
According to Raoul Manalac, MD, the senior director of obesity science at Ro, the remote care platform can help enhance patient-provider communication, especially for folks who'd otherwise go without patient engagement.
"Ro's platform makes it easy for patients or providers to connect, enabling patients to ask a question, report a side effect or share progress with a provider any time they need," Manalac said in an emailed statement. "This means that patients can more conveniently connect with their provider throughout their journey -- helping them to effectively reach their health goals."
The Body Program from Ro is a $145 monthly subscription for patients. Patients fill out a questionnaire and consult with Ro providers about treatment goals and clinical needs. If appropriate, the provider will write a prescription for a branded GLP-1 drug or a compounded semaglutide. While Ro does not cover the cost of the drug, it does offer a concierge tool to help the patient obtain insurance coverage.
Patients also have the option to forego insurance and pay out-of-pocket for the medication.
From there, the remote care company seeks to support patients in their clinical journeys using digital tools, like patient messaging and prompted, automated check-ins.
"Every patient benefits from ongoing access to personalized care and support at each step of their care journey," Manalac explained. "The Body membership combines access to medication along with everything needed to help make it most effective, including expert provider care, 1-1 coaching from nurses, progress and side-effect tracking, and an educational curriculum that covers lifestyle, nutrition and exercise topics."
Although Ro offers a subscription membership model and concierge services to navigate insurance, Manalac said its patients aren't immune to the drug shortages and skimpy coverage affecting patient adherence to GLP-1s.
"Throughout our experience helping patients across the country, we've unfortunately witnessed how much GLP-1 shortages can be a barrier that affects continuity of care and adherence to treatment," Manalac explained.
However, the company does see on-demand technology as a tool to help navigate shortage woes.
Earlier this year, Ro launched the GLP-1 Supply Tracker, an open-access tool set up to help patients and providers keep track of which GLP-1 medications are in stock and which are in shortage. Although the tool doesn't chip away at the shortage problem, it provides insights to patients and providers working to obtain access to the medications.
With GLP-1 access and adherence on such shaky ground, obesity and diabetes experts are doubling down on the perils of taking the medications without a comprehensive engagement system backing them up.
In the next part of this two-part series, we'll discuss the cultural and industry forces that challenge wraparound patient engagement for GLP-1 management and the way the nation's evolving views on obesity confront those challenges.
Sara Heath has covered news related to patient education and health equity since 2015.






