
Getty Images/iStockphoto
How Will MACRA Impact Patient Engagement, Care Coordination?
As the first reporting period draws nearer, providers will need to understand the patient engagement requirements listed under MACRA.
In 2015, Congress passed the Medicare Access and CHIP Reauthorization Act (MACRA) with an overwhelming bipartisan majority. The complex piece of legislation has a number of provisions, each of which affects different areas of the healthcare industry, including patient engagement.
MACRA includes two major components: the Merit-based Incentive Payment System (MIPS) and incentive payments for alternative payment models (APMs). Both contribute to the industry’s overall emphasis on patient engagement, care coordination, and more collaborative care.
Patient-centered care is one of the primary goals of CMS.
In its proposed rule, which was published in April of 2016, CMS explained that it created both the APM requirements and MIPS to drive patient-centered healthcare and continue the development of patient engagement as a fundamental component of healthcare.
“By incentivizing participation in certain APMs, such as Accountable Care Organizations (ACOs), Medical Home Models, and episode payment models, and by incentivizing quality and value for eligible clinicians under the MIPS, we support the nation’s progress toward achieving a patient-centered health care system that delivers better care, smarter spending, and healthier people and communities,”CMS said.
CMS has added in patient engagement requirements to MIPS through Advancing Care Information, one of the four components contributing to the MIPS score. The agency also emphasizes patient-centered care through its APM incentive payments, as robust engagement is one of the driving factors toward APM success.
Below, PatientEngagementHIT.com breaks down the patient engagement provisions included in MACRA, highlighting the effect of the legislation on patient-centered healthcare going forward.
Dig Deeper:
- What is MACRA and What It Means to Providers, EHR Technology
- Proposed MACRA Rule to End Meaningful Use for Physicians
Advancing Care Information
Advancing Care Information, which accounts for 25 percent of the MIPS score, is the replacement for meaningful use for eligible providers. It is also the portion of MIPS which houses the patient engagement requirements.
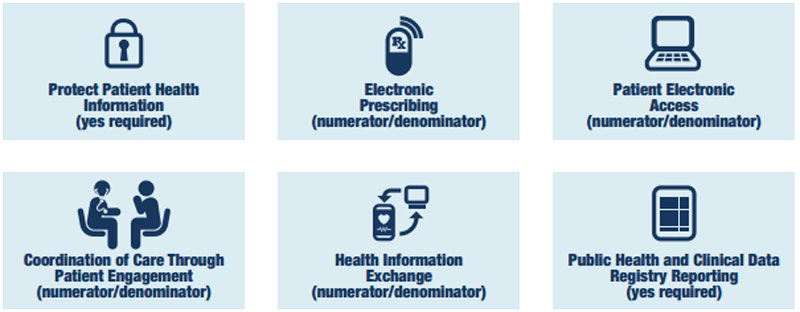
Advancing Care Information is scored on a 0-100 point scale. This scale includes a base score of 50 points, which requires either a yes/no answer for the proposed objective measures or a report on a calculated numerator and denominator

The performance score allows providers to earn up to 80 points. Providers have the opportunity to score over the 100-point threshold. All providers who score 100 points or more will receive the full 25 percent of the MIPS score.
Both the base score and the performance score include specific objectives for patient engagement, including patient access to health data and care coordination through patient engagement.
Dig Deeper:
Patient engagement through health data access
The Advancing Care Information program will include objective measures requiring patient access to health data. There are two measures under this umbrella objective:patient access requirements and patient-specific education requirements.
Patient electronic access to health data will be a numerator and denominator score. Providers will submit the number of patients it has allowed access to their health data in the numerator, and the number of total patients seen in the denominator.
Eligible providers must offer the ability to view, download, or transmit health data to their patients, and engage at least one patient per reporting period. The eligible provider must also ensure that this data is available to the patient via the device of their choice using an API.
Patient-specific education measures require providers to identify areas of education that may aid patients with chronic disease management, treatment decisions, or other needs, and to offer electronic educational materials to at least one unique patient per reporting period.
Dig Deeper:
- How Patient Health Data Access Drives Patient Engagement
- Top 3 Challenges Limiting Patient Access to Health Data
Patient engagement and care coordination
There are three measures under the care coordination objective umbrella, including view, download, and transmit requirements, secure messaging requirements, and patient-generated health data requirements.
View, download, and transmit requirements can be fulfilled via the following three methods:
- Viewing, downloading, or transmitting data to a third-party
- Accessing health data through an API
- A combination of the two options
The secure messaging measure requires at least one unique patient to receive at least one secure direct message over the physician EHR. Eligible providers may also fulfill this requirement by responding to a patient query via direct message.
The patient-generated health data requirements ask providers to incorporate data contributed by the patient from at least one unique patient.
The care coordination through patient engagement requirements all contribute toward the goal of putting the patient at the center of healthcare.
Through the patient engagement strategies required in MIPS, patients are put in control of their health data and may help bridge communication gaps between different providers.
Secure direct messaging functions may be useful for coordinating care not only between different providers, but between patient and provider. These communication strategies are ideal for answering patient questions or reminding them of treatment protocols, helping to recognize the patient as an integral member of the care team.
Patient-generated health data likewise integrates the patient as a member of the care team. Engaging patients in data aggregation may be helpful for boosting empowerment.
Dig Deeper:
- 3 Benefits of Patient-Generated Health Data, Patient Engagement
- How Secure Direct Messaging Lowers Out-of-Pocket Patient Costs

APMs and patient engagement
Alternative payment models (APMs) are the second leg of the MACRA legislation. Should a provider not participate in MIPS, she must participate in an eligible APM. Examples of APMs include certain accountable care organizations, patient-centered medical homes, and bundled payment models.
These value-based care models rely on comprehensive care approaches. In order to care for the whole patient, those participating in a value-based care model must utilize different patient engagement strategies.
Research shows that patient engagement in an ACO centers largely on communication and education for the patient.
“Because patients may not enroll in the ACO per se (eg, in a Medicare ACO) but instead become involved in the ACO by virtue of where they receive primary care, patients may not associate or identify with ‘their’ ACO itself,” said researchers from the Agency for Healthcare Research and Quality (AHRQ).
Because of this, ACOs must foremost educate their patients on the care model, explaining the benefits and details of how it will function to keep them healthier.
ACO leaders also need to practice population health management that will help them identify those who they will serve in the ACO.
ACO beneficiaries are often determined by geographic location, patient demographics, or chronic disease status. By identifying these populations and determining their needs, providers can better serve them and potentially see more success with the care model.
Last, providers participating in an ACO must work to forge genuine relationships with their patients, helping to serve their needs inside and outside of the practice. Through better interpersonal communications and feedback collection, providers can improve their relationships with beneficiaries and caregivers.
Patient-centered medical homes – which aim to deliver patient-centered care through care coordination, preventative services, population health management, and extended access to care services – likewise thrive off robust patient engagement.
According to AHRQ, PCMHs can drive patient engagement through three strategies:
- Patient involvement in their own care
- Quality improvement in the primary care practice
- Policy and research development and implementation
Many healthcare experts consider patient engagement a critical component of patient-centered medical homes. Through efforts to improve medication adherence, preventative and primary care, and healthcare access, PCMH leaders must deploy robust patient engagement strategies.
“Involving patients in the medical home is seen by some stakeholders as intrinsically valuable and as a model of care that should be pursued regardless of whether it lowers costs or improves health outcomes,” AHRQ says.
By extending healthcare to underserved populations, engaging patients in healthy lifestyle changes, and maintaining adherence to treatment protocols, providers may consider patient engagement strategies to ensure their PCMHs are effective.

MACRA reporting considerations and flexibilities
Leading up to and following the proposed MACRA rule, many industry groups – including the American Hospital Association and the American Medical Association – spoke out against the program’s timeline. Stakeholders said the program’s timeline was too arduous given the proposed start date of January 1, 2017.
By mid-July of 2016, CMS Acting Administrator Andy Slavitt was reportedly considering changes to MACRA’s timeline, and by the end of September the agency had taken action.
In a September blog post, Slavitt detailed a new “pick your pace” policy for MACRA reporting, which gives providers four options for reporting to the Quality Payment Program (QPP), which is how CMS refers to the overall MACRA framework and other provisions included in the legislation.
The first option requires providers to simply submit what data they have during the 2017 reporting period as a way to ease slowly into QPP participation. Providers who select this option will not see positive payment adjustments, but they will be able to avoid the negative payment adjustment.
The second option allows providers to submit quality data for less than a full calendar year. Providers could begin submitting data after the January 1 start date and still qualify for a small positive payment adjustment.
The third option allows providers to participate in the program for the full calendar year, meaning they are ready to begin on January 1, 2017. These providers would submit reports on quality measures, technology use, and practice improvements. These providers could quality for a “modest” positive payment adjustment.
The final option is for providers to fully participate in an Advanced Alternative Payment Model, such as a Medicare Shared Savings Program (MSSP) track level two or three. Should a provider receive enough of her Medicare payments or see enough Medicaid patients within this model, she may qualify for a 5 percent payment adjustment.
According to Slavitt, CMS made these changes following feedback stating that MACRA’s timeline may detract from quality patient care. Keeping in line with the agency’s commitment to more patient-centered care, Slavitt said CMS worked to make feasible and effective adjustments to the schedule.
“We heard from physicians and other clinicians on how technology can help with patient care and how excessive reporting can distract from patient care; how new programs like medical homes can be encouraged; and the unique issues facing small and rural non-hospital-based physicians,” Slavitt wrote in the blog post.
“We wanted to share our plans for the timing of reporting for the first year of the program. In recognition of the wide diversity of physician practices, we intend for the Quality Payment Program to allow physicians to pick their pace of participation for the first performance period that begins January 1, 2017.”
How the industry is responding to MACRA’s patient engagement rules
Many stakeholders have taken a positive view of the patient engagement and care coordination provisions included in the new payment program.
At the National Partnership for Women & Families, experts say MACRA is an “encouraging first step for patient-centered care.”
“MACRA’s Quality Payment Program has the potential to be a catalyst for changing how our nation pays for health care and moving us away from fee-for-service and toward value-based payment,” said National Partnership president Debra L. Ness in a comments letter.
“But to be successful, CMS and participating providers must give as much attention to improving the delivery of care as they do to reducing spending.”
The National Partnership advised CMS to add in provisions to the Advancing Care Information portions of the law, calling for even more patient engagement protocol. These may include requiring providers to identify how they will use health IT to improve patient-centered care.
The National Association for Trusted Exchange likewise praised the law, noting the positive influence patient access to health data will have on the industry.
“NATE is pleased to see that CMS is poised to reward providers for increasing their options for achieving electronic communication with their patients,” the group said in a public statement.
“The proposed MACRA Advancing Care Information (ACI) performance category’s base score determination not only requires that providers demonstrate that they can share information with their patients through secure messaging, it also requires providers to allow patients to access their own information using any consumer-facing application (CFA) of their choice through an API.”
Going forward, providers will need to prepare for these patient engagement requirements under MACRA in order to successfully participate in the program. Through the requirements under MIPS and the emphasis placed on APMs, providers reporting on MACRA may be able to help propel the healthcare industry into a future of patient-centered healthcare.
Dig Deeper:







