
Getty Images
PCPs Lack Time, Tools to Address Social Determinants of Health
Family physicians are struggling to find the time to address social determinants of health, but the AAFP is offering new resources to help them.
Family physicians recognize the important role that the social determinants of health play in managing population, but lack the time, tools, and resources to have meaningful conversations with their patients, according to a recent survey from the American Academy of Family Physicians (AAFP).
Eighty-three percent of family physicians (FPs) agree that the social determinants of health, including housing and food security, community safety, access to transportation, and health literacy, have a significant impact on patient outcomes and should be addressed.
More than three-quarters of the nearly 500 AAFP members participating in the survey added that collaboration with community organizations will be key to understand and addressing social determinants that affect their patient populations.
Yet 80 percent feel as if they do not have the time to discuss these important circumstances with their patients during routine consults, and 64 percent of providers don’t believe they have the staff or resources to do anything about these risk factors even if they can identify them.
The AAFP has started to develop a provider toolkit called The AAFP's The EveryONE Project aimed at reducing the disconnect between the number of providers who acknowledge the importance of socioeconomic factors and the number of physicians equipped to manage them.
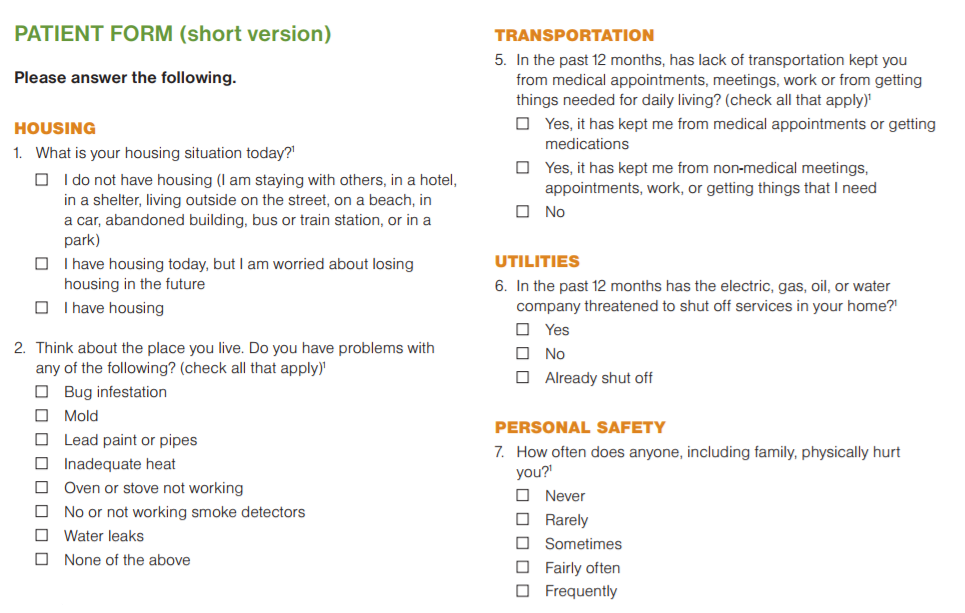
The freely available resources include patient screening tools and printable assessments that address key socioeconomic concerns.
The assessments including questions about housing quality, such as whether the patient’s home has working smoke detectors, leaking water pipes, mold, or insect infestations, as well as questions about interpersonal violence and abuse, utility access, secure access to food, and whether or not the patient would like assistance with one or more of these concerns.
“During the toolkit's development, we realized that as the importance of the issue continues to grow and the practice of SDOH screening becomes more common, there will be additional demands on the AAFP to go further than just providing a screening toolkit as a patient-level intervention," said Danielle Jones, MPH, manager of the AAFP's Center for Diversity and Health Equity (CDHE), which is overseeing The EveryONE Project.
The resource package also includes a guide for providers detailing how to integrate social needs assessments into a team-based primary care practice.
The guide suggests that receptionists or medical assistants can distribute the short-form 11-question assessment upon a patient’s arrival, while a nurse, physician assistant, or health educator can review the patient’s answers and begin to plan any necessary counseling or referrals.
A longer-form questionnaire with additional questions about child care, education, finances, and transportation is also available.
“Screening for SDOH does not need to be administered by a physician, and it can be performed upon check in or while rooming so that it does not disrupt the flow of the visit while promoting more comprehensive care,” the guide states. “The screening tool can be self-administered or given via an in-person interview. However, individuals may be more likely to disclose sensitive information, such as interpersonal violence, when self-administered.”
Physicians may not need to administer the questions themselves, but they should still participate in reviewing the patient’s answers, the document adds.
Patients may feel more comfortable discussing sensitive issues with a physician they know and trust, and as leaders in the team-based care format, physicians may be in the best position to refer the individual to the correct member of their care team.
As the accompanying survey pointed out, the majority of providers may struggle to allocate the time and resources to fielding and acting upon even short patient assessments.
An integrated social worker or community health worker can certainly be an important asset for organizations with the budgets to launch such programs, but the AAFP stresses that there are numerous free resources available to help providers understand their local needs and identify existing services to work with higher-needs populations.
The 211 Helpline Center, available in regions in all 50 states and Puerto Rico, allows users to call – or in many cases connect by text message – to access crisis services and basic needs resources such as meal access for children, utilities assistance, information on eligibility for social care programs.
Providers can also get a sense of what resources and partnerships might be most impactful to prioritize for their populations by using the Robert Wood Johnson Foundation’s County Health Rankings and Roadmaps tool.
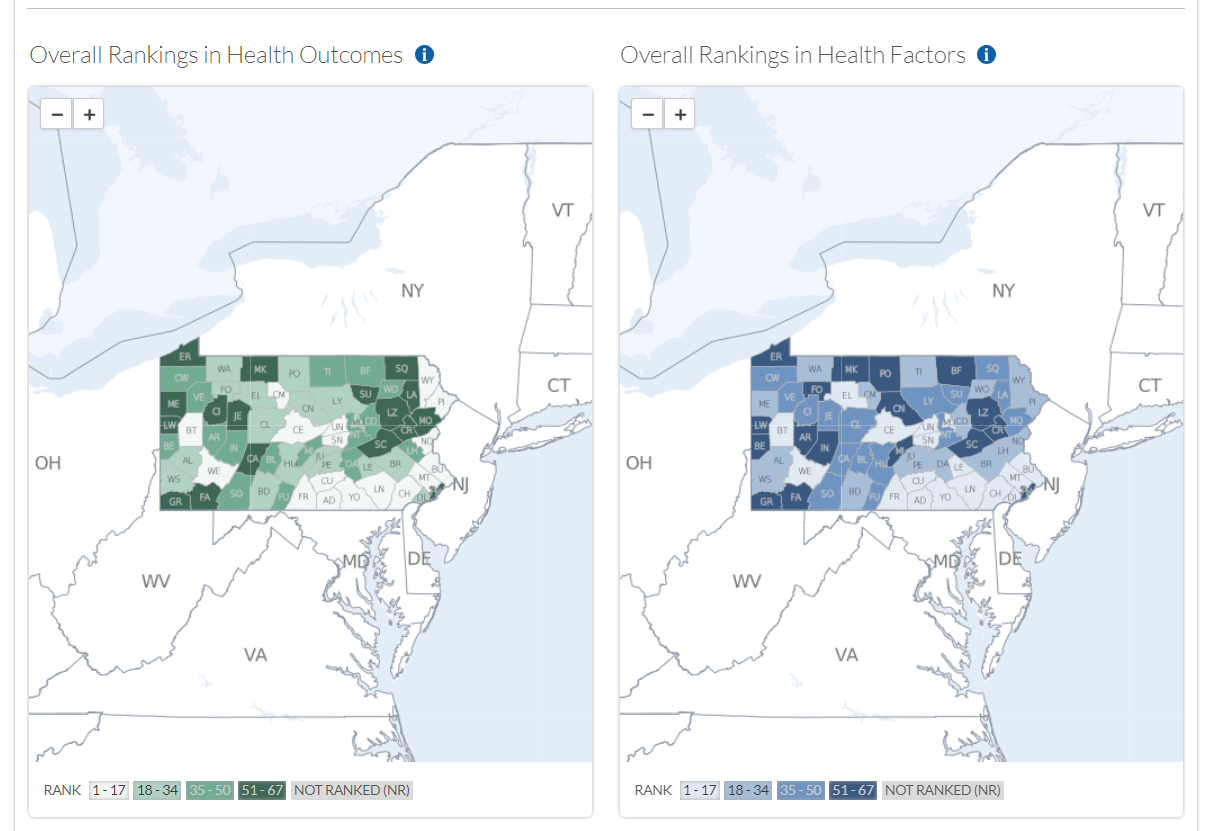
The interactive online map breaks down the socioeconomic landscape county by county, offering insights into health outcomes as well as the health factors that contribute to them. The tool includes lifestyle behaviors, such as smoking, excess alcohol consumption, and obesity rates, as well as statistics about care access, education and employment rates, and poverty levels.
For many counties, information about the physical environment is also available. Data includes air pollution levels, recent drinking water quality violations, severe housing problems, and how long it takes individuals to commute to work.
Stakeholders can also connect with a Community Coach who can help break down the data or suggest activities to help address the needs of vulnerable populations.
The AAFP plans to release even more population health management resources in 2018, including a community-level social determinants of health toolkit that will be available in March.
The kit will allow providers to assess their readiness to start addressing socioeconomic needs for more of their patients and tips for developing partnerships with community organizations and behavioral healthcare providers.
"You can also look to the CDHE to begin communicating its work more broadly, not just across the family medicine specialty, but also with other industries and sectors to develop high-impact collaborative partnerships aimed at advancing health equity,” Jones said.






