
Olivier Le Moal - stock.adobe.co
The Role of Healthcare Data Governance in Big Data Analytics
What does data governance mean to healthcare organizations and why is it so crucial to master before engaging in big data analytics?
Data has always been the lifeblood of the healthcare industry. From blood pressure readings and surgical records to insurance claims, immunization histories, patient demographics, and payment receipts, every action of every member of the healthcare ecosystem relies on an endless stream of information.
Before the advent of the electronic health record, the vast majority of this data was trapped in file folders and banker’s boxes. This static data resource, often obscured by illegible handwriting, missing papers, and mistakenly misplaced records, was of little use to data scientists seeking innovative ways to leverage history to predict the future of patient care.
As the industry reluctantly adopted EHRs, stakeholders started to explore the new frontier of big data analytics. Driven by the prospect of payment reforms that promote quality over quantity, providers began to clamber for automated tools to help them understand clinical risk, communicate with their patients more effectively, and perform the population health management tasks that will help them succeed in a new financial landscape.
But when it comes to big data, old habits die hard. The haphazard data governance practices that made paper records such a nightmare were often magnified, not ameliorated, by the switch to an electronic environment.
Convoluted and unintuitive EHR interfaces made data entry an immensely frustrating task for overwhelmed clinicians. Health information managers struggled to walk the line between the benefits of structured templates and their inability to capture the full story of the patient. Technical experts often took a slapdash approach to EHR optimization, fixing problems however and whenever they could without necessarily thinking about the long-term implications.
Many healthcare organizations are still struggling through this hectic phase of the big data adoption cycle, and they often feel as if they simply do not have the time, the money, or the resources for a concerted effort to make data governance a priority.
A 2015 survey by the American Health Information Management Association (AHIMA) found that nearly a third of participants have made no headway in promoting data governance as a business imperative, and another 24 percent added that governance is simply not a priority for their leadership.
But ignoring the role of data governance in the big data environment may be penny wise, pound foolish. Without robust, accurate, timely, clean, and complete data, healthcare organizations will not be able to move beyond the basics of record keeping and develop the analytics competencies that will become vital survival skills in the emerging world of value-based care.
What is data governance? Is it the same as information governance?
“Data governance” and “information governance” are two common terms that are often used interchangeably, but differ in significant ways.
Data governance is the practice of managing data assets throughout their lifecycle to ensure that they meet organizational quality and integrity standards. Data governance is geared towards making sure that users can trust their data, which is especially important when making patient care decisions.
As part of a comprehensive data governance program, users are held accountable for creating high quality data and using that data in a secure, ethical, authorized manner.
In the healthcare industry, health information management professionals are often responsible for developing and overseeing data governance principles that improve the consistency, reliability, and usability of data assets while optimizing EHR interfaces to eliminate unnecessary or duplicate steps for end-users and eradicate problematic workarounds.
The goal of these activities is to improve staff efficiency, foster an environment of accountability, and create a standardized, interoperable pool of big data that can be used for organizational improvements and higher quality clinical decision-making.
Information governance is slightly different, according to AHIMA, but it is closely linked to data governance.
AHIMA defines information governance as “an organization-wide framework for managing information throughout its lifecycle, and for supporting the organization’s strategy, operations, regulatory, legal, risk, and environmental requirements.”
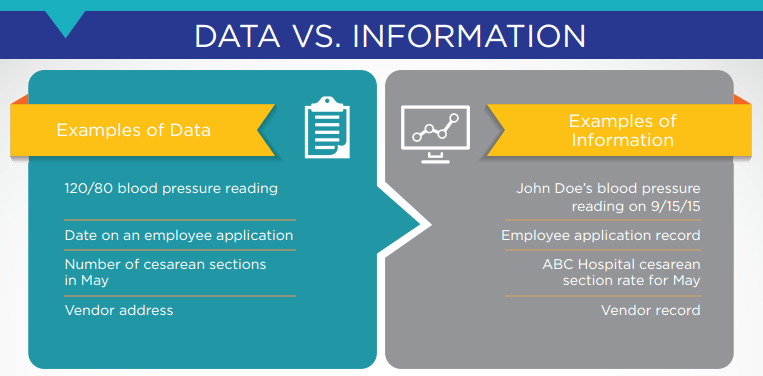
Information is the result of combining multiple pieces of data to create an insight. A single data point, such as one blood pressure reading without any additional context, imparts little meaning on its own. But a series of readings over the past two years of a patient’s life can show that the patient’s blood pressure is trending upward at a worrying rate.
A clinician may wish to use this knowledge to prescribe a medication, advise the patient to change his lifestyle, or take some other step to address the situation. That is how data becomes actionable information for decision-making.
The complementary nature of data governance and information governance is especially critical for organizations that are hoping to engage in big data analytics, since each individual data set must be clean, accurate, standardized, and comprehensive before it can be combined with additional data sources to produce actionable insights.
How to Choose the Right Healthcare Big Data Analytics Tools
What is EHR Optimization and How Does It Start?

How do data governance and information governance impact a healthcare organization?
Data and information underpin nearly every activity within a healthcare organization, but some areas of operations and clinical care depend on robust data integrity and governance more than others.
Patient safety is a top priority for every provider, and poor data governance can quickly create critical problems. From the moment a patient sets foot in the office or consult room, his or her data must be accurately identified and must follow the patient throughout every interaction.
However, even the basics of matching a patient to the correct record is not as easy as it seems without a quality data governance approach. More than half of health information managers encounter patient matching issues on a frequent basis, most of which must be manually addressed.
Duplicate records and inappropriately merged records from separate individuals are among the top threats to patient safety.
“Severe patient-care issues can occur and resources are wasted when systems are inundated with duplicate records,” AHIMA said. “Patient safety is a major concern for many organizations, yet it is necessary to increase awareness of the safety, legal, financial, and compliance concerns created by duplicate and overlaid medical records.”
Even if the right record is paired with the right patient, safety and care quality may suffer if that record is incomplete, incorrect, or outdated. Missing or incorrect data about allergies, current medications, past procedures, and health conditions can drastically impact the course of treatment, and may create opportunities for harm.
EHR data integrity shortfalls routinely feature on industry patient safety hazard lists, and may add to the frustrations of clinicians already wrestling with electronic interfaces that compound their data entry problems and may lead them into sub-optimal practices.
Documentation cloning remains a thorn in the side of health information managers who worry about the replication of outdated or incorrect data throughout the patient record. A 2013 survey found that more than three-quarters of clinicians routinely copied and pasted information across fields within their EHRs, which not only reduces the usefulness of the software, but may expose organizations to fraud charges.
Just this month, Kentucky-based home health provider MD2U was required to pay several million dollars to the federal government after being accused of upcoding and improper documentation cloning.
“The ability to migrate notes from visits that occurred weeks, months, or even years prior to the current patient encounter created the illusion that MD2U’s non-physician providers (NPPs) were performing a significant amount of work during their patient encounters when, in fact, they were not,” explained the Department of Justice.
“If the documentation was deficient to bill the highest level code, MD2U would direct NPPs to go back and change the medical record — after the encounter had occurred — to falsely show that more work was performed during the visit in order to support the highest level billing.”
This is clearly an extreme case of data governance gone wrong, but it serves as a cautionary tale to other providers who may be opening themselves up to negative outcomes due to inattention to data integrity and governance.
Data governance is also crucial for big data analytics, population health management, performance improvement benchmarking, and reporting for regulatory programs such as meaningful use.
A strong governance program not only makes clinical care easier and more reliable, but will allow organizations to prepare for future analytics projects in an increasingly complex environment, said Deborah Green, MBA, RHIA, Executive Vice President and Chief Operating Officer of AHIMA.
“Sometimes we feel like we’re drowning in data, but the challenge isn’t just the volume. It’s the integrity and the quality of that data,” she stated at the organization’s 2015 convention.
“We need information governance to enable trust. What will that buy us? Each organization will be able to trust their data for key decision making and be confident enough to leverage that information to promote themselves.”
“Sometimes we feel like we’re drowning in data, but the challenge isn’t just the volume. It’s the integrity and the quality of that data."
Improved data governance, coupled with the growing importance of clinical quality measures for reporting and benchmarking, will be key for driving overall systemic improvement, as well, added National Quality Forum President and CEO Christine Cassel, MD.
“Everybody needs and deserves to have consistent and accurate information about healthcare,” she said to HealthITAnalytics.com. “That’s easy to say, but in a world where data sources are multiplying by leaps and bounds and where there’s a growing emphasis on tying payment to performance, there’s a lot of complexity when it comes to actually implementing systematic improvements.”
“Some of those challenges have to do with understanding big data in every way it manifests itself,” she continued. “We always have to ask ourselves how we can turn data into meaningful information, particularly for consumers and providers. You do that by creating measures that are accurate and that are consistent so that you can compare apples to apples across a community, a group of providers, or across the nation as we try to achieve the Triple Aim of better population health, better healthcare, and more affordable healthcare.”
Balancing Access and Insight for Healthcare Big Data Analytics
Can Big Data Analytics, Data Governance Restore Joy to Medicine?
How can healthcare organizations begin to develop a meaningful data governance strategy?
The first step for developing a data governance plan is recognizing the need for one at the very highest level. Healthcare organizations that commit to making governance a top priority on every rung of the corporate ladder are more likely to see success, and to adequately support their health information management staff during the process.
Enlisting the participation of organizational leaders can jumpstart the development of a cross-departmental information governance team, which should include HIM experts, EHR optimizers and technical staff, physician and nurse champions, financial leadership, and big data analysts.
Providers should clearly define their information governance goals and create measurable benchmarks to gauge executed progress. Each member of the governance team should have a set of well-understood tasks and responsibilities, and should be given the opportunity to provide input, listen to feedback from their peers, and work across departmental lines to achieve their objectives.
“Everybody needs and deserves to have consistent and accurate information about healthcare.”
AHIMA suggests that organizations conduct an information governance gap analysis to identify pain points in the data creation, storage, analysis, and reporting process. Providers should pay special attention to areas of concern that may directly impact patient safety, privacy, and compliance issues in order to avoid serious adverse events.
A 2013 report by researchers from Kaiser Permanente, the University of Pennsylvania, and several public health institutes also recommends that healthcare organizations create a set of guiding data governance principles that fit the mission, vision, and values of the particular provider.
When creating specific policies and procedures, providers should pay close attention to “accountability, authority, roles, rules of engagement (how people work together), management of cross-functional conflicts, decision making and rights, stewardship, management of change, resolution of issues, making and enforcing rules, management of cost and complexity and creating value.”
These principles should be communicated clearly across the organization, and members of the data governance leadership team should take the time to explain the project in detail to staff members, answer any questions, and ensure widespread buy-in for improvement activities.
After outlining a strong vision and laying the foundations of data governance, organizations may wish to begin a clinical documentation improvement (CDI) program to train end-users on the importance of creating good data from the start.
While clinical documentation improvement received a great deal of attention in the run-up to ICD-10 implementation, its value goes far beyond capturing the data required to code claims appropriately.
Not only does improved documentation help to smooth the financial side of the healthcare business, but it ensures that providers are capturing all the data necessary to accurately report their own performance and clinical quality. This is become increasingly important as reimbursement becomes more and more dependent on reported patient outcomes.
Healthcare organizations should also include opportunities for continued monitoring and ongoing improvement as they create their data governance strategies. End-users should receive regular training and reminders about optimal data integrity and data entry practices, and organizations should conduct frequent internal audits and assessments to ensure they are maintaining a high level of data quality.
These activities will ensure that healthcare providers are prepared to utilize their growing big data resources for generating actionable insights, and that they are being mindful of patient safety and care quality as they optimize their assets for the future of value-based care.
Why Is CDI Important for Clinical Analytics, Data Integrity?
Four Ways to Boost EHR Data Integrity for Big Data Analytics






