
Getty Images
Breaking Down the Basics of the Patient-Centered Medical Home
The patient-centered medical home offers a step-by-step roadmap for care quality improvements that align with larger reform efforts, but not everyone is sold on its value just yet.
As the healthcare industry moves away from traditional fee-for-service reimbursements towards a new era of accountable, cost-conscious, coordinated care, healthcare organizations are actively seeking new patient management strategies to meet stringent quality and spending goals.
Managing chronic diseases, reducing unnecessary utilization, maintaining wellness, and involving patients in their own care are top goals for the healthcare system, and the patient-centered medical home (PCMH) model has quickly become one of the most popular frameworks for achieving these objectives in an organized manner.
This comprehensive care strategy, often backed by certification from the National Committee for Quality Assurance (NCQA) or another accreditation body, stresses a patient-centered approach to care coordination, population health management, preventative services, health IT utilization, and expanded accessibility.
But the healthcare industry is divided over whether or not the time, commitment, and financial investment involved in PCMH adoption will really return meaningful results.
Do providers have the resources to overcome the initial start-up costs, stick with the program, and achieve better outcomes for their patients? How long will it take, and what steps are required? What are the benefits of undertaking this comprehensive practice transformation?
What is the patient-centered medical home model?
The patient-centered medical home is a series of guidelines and best practices intended to foster more complete, accessible, and data-driven preventative care and patient management.
According to the 2007 Joint Principles of the PCMH, created by a number of primary care professional societies, the PCMH is based on five pillars of coordinated care:
- Taking the whole patient into account by delivering comprehensive physical and behavioral healthcare through a team-based network of providers
- Developing meaningful relationships with patients, caregivers, and family members that take into account the patient’s cultural values and preferences, as well his or her socioeconomic experiences
- Employing coordinated, data-driven care strategies fueled by electronic health record (EHR) use, health information exchange (HIE), data analytics, and population health management tools
- Ensuring care access by expanding office hours, employing telehealth or other remote communications technologies, offering same-day appointments for pressing needs, and educating patients about alternative care sites for emergencies
- Placing a premium on care quality and patient safety by leveraging clinical decision support technologies, clinical guidelines, and alerts that flag potential gaps in care
Providers looking to obtain recognition under one of the industry’s PCMH programs will need to meet detailed objectives under each of these categories, which include activities such as providing treatment plans and educational materials to a certain number of patients or choosing a set of chronic diseases to monitor using population health management technologies.
These activities align closely with the broad goals of other healthcare reform efforts, such as meaningful use, MACRA, and accountable care organizations.
However, the PCMH does not include any reimbursement requirements or financial risk. It is simply a useful checklist for adhering to best practices and designing workflows that foster quality care.
While healthcare organizations may choose to adopt some, most, or all of the PCMH principles without seeking accreditation from the NCQA or other PCMH certification organization, many providers choose to apply for recognition of their transformation.
As health IT adoption becomes nearly ubiquitous among providers, PCMH regulations have changed to more or less require the use of EHRs and other population health management tools to generate reports, monitor patients, and coordinate care.
Understanding the Basics of the Patient Centered Medical Home
Using Health IT to Support the Patient Centered Medical Home
What are the expenses and commitments involved in practice transformation?
The patient-centered medical home promises improvements in care, but not without some costs. Some recent studies have warned that getting a PCMH off the ground can be prohibitively expensive for cash-strapped providers, since many of the transformation costs must be paid up-front.
A recent RAND Corporation study found that PCMH transformation costs could pile up to anywhere between $83,829 and $346,603 per annum during a process that could take several years.
Based on data from the Pennsylvania Chronic Care Initiative, the RAND report found that the costs per clinician ranged from $18,585 to $93,856, with the median costs weighing in at $147,573 per practice and nearly $65,000 per clinician.
A similar report from September of 2015 said that the staffing and care coordination requirements of the PCMH could sap an average of $8600 per month from healthcare organizations – and smaller providers may be particularly susceptible to racking up big bills.
Long-term commitment is also a core requirement of PCMH transformation, and the journey to coordinated care can be arduous. A CMS Innovation Center pilot program for federally qualified health centers (FQHCs) found that it took longer than anticipated to complete the PCMH transformation, and that there was little to no evidence available that the program produced gains in effective care.
Adding to the argument that the framework may not be an attractive option for everyone, maintaining a PCMH certification can be just as difficult as achieving it.
In an op-ed published in 2015 by the Annals of Family Medicine, Dr. Edward Bujold from North Carolina detailed the difficulties of meeting one of the PCMH’s most ambitious requirements: demonstrating continuous improvement in order to receive recertification.
“In the past year alone, my staff and I spent hundreds of hours studying for and taking exams, certifying for numerous programs, and updating then relearning our EHR to meet meaningful use requirements,” he wrote.
“This was time we could have spent in patient care or pursuing outside interests designed to nurture our physical and mental wellbeing—the fourth pillar of the Quadruple Aim: improving the health of populations, enhancing the patient experience, reducing the per capita cost of health care, and improving the work life of health care providers, including clinicians and staff.”
ACO, PCMH Models May Not Be Boosting Care Quality, Satisfaction
Is Maintaining the Patient-Centered Medical Home Worth It?
What are some of the positive results of adopting this framework?
But not every PCMH participant has soured on the experience. In fact, many of the case studies about PCMH adoption strike a decidedly positive tone. The costs may be unavoidable, but the rewards are likely to be worth it, argues the Patient-Centered Primary Care Collaborative (PCPCC), among others.
“The financial aspect has been an ongoing challenge,” acknowledged PCPCC CEO Marci Nielsen, PhD, MPH. “We’ve got somewhere in the neighborhood of 15 to 20 percent of practices adopting this model because they know it’s good for patients, but the last 80 percent are still holding out for payment reform. It’s not because they’re obstinate. More often than not, they literally just can’t afford to make changes to their practice without some upfront funding.”
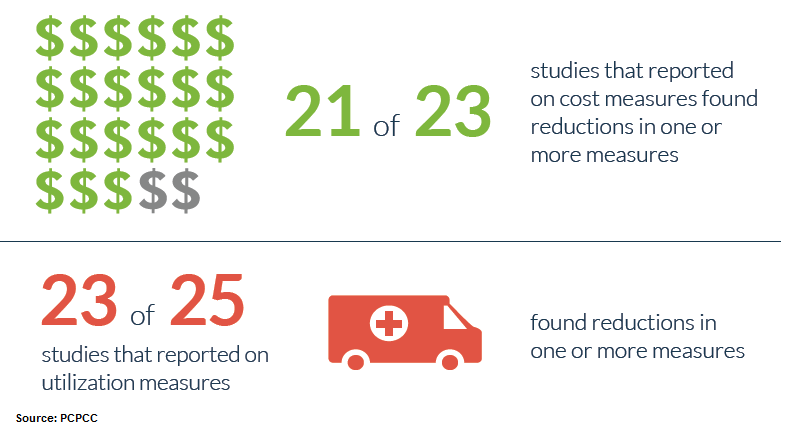
Providers that do make the leap often see significant results, however. The most recent annual report from the PCPCC states that 91 percent of studies about PCMH costs and spending showed cost reductions under the framework. Twenty-three out of 25 reports on utilization found that providers improved their performance on at least one measure.
Many of the case studies boast double-digit gains in hospital readmissions, emergency department utilization, and spending on inpatient care. Payers have achieved hundreds of millions of dollars in cost savings by leveraging the PCMH, and providers have earned tens of thousands in performance bonuses when the model is tied to hitting quality targets.
In contrast to Dr. Bujold’s frustrations, Pam Minichiello, Project Director at the Massachusetts eHealth Collaborative (MAeHC), believes that slow and steady progress towards PCMH goals is a sustainable way to achieve savings and raise quality.
“I think that anybody can do it,” she said. “Is it easier for some organizations rather than others? Yes, absolutely. But it really is dependent upon their commitment to the process and what their drivers are. It does take resources.”
“But it also drives efficiency within the practice. It increases patient satisfaction, overall performance, as well as population health management. It’s so important to use these models to meet the challenges that are going on right now in healthcare.”
How the Patient-Centered Medical Home “Repackages” Primary Care
Patient-Centered Medical Home Is a “Pragmatic” Shift in Care
Why is the patient-centered medical home important in light of recent healthcare reforms?
While the jury is still out for many providers when it comes to the ultimate worth of the PCMH model, the debate is about to take an interesting turn. Under the new MACRA legislation, certain patient-centered medical home programs qualify as Advanced Alternative Payment Models (APMs) that may allow providers to avoid attestation under the Merit-Based Incentive Payment System (MIPS).
“A patient-centered medical home will be recognized if it is a nationally recognized accredited patient-centered medical home, a Medicaid Medical Home Model, or a Medical Home Model,” states CMS in the proposed MACRA rule published in the Federal Register.
“The NCQA Patient-Centered Specialty Recognition will also be recognized, which qualifies as a comparable specialty practice. Nationally recognized accredited patient-centered medical homes are recognized if they are accredited by: (1) The Accreditation Association for Ambulatory Health Care; (2) the National Committee for Quality Assurance (NCQA) PCMH recognition; (3) The Joint Commission Designation; or (4) the Utilization Review Accreditation Commission (URAC).”
Most of the healthcare industry is still puzzling through the 900-page MACRA documentation, trying to figure out which pathways are best suited to their particular needs. But providers who have achieved one of the approved PCMH designations may be ahead of the pack when it comes to successfully navigating this new landmark effort.
With its emphasis on coordinated care, patient engagement and satisfaction, team-based decision making and communication between providers across the care continuum, the patient-centered medical home is a valuable tool for healthcare providers looking to take an innovative approach to practice transformation.
How Does an ACO Differ from the Patient-Centered Medical Home?





