Getty Images/iStockphoto
Unnecessary Utilization in CO Leads to $134M in Healthcare Spending
The share of healthcare spending on low-value care was highest in Colorado’s commercial health plans.
Updated 8/24/2023: This article has been updated to reflect that the share of healthcare spending on low value care was highest in commercial health plans. Previously, the article framed Medicaid and CHP+ as having the highest spend due to a misreading of certain nuances in the source material. Some of the wording has been changed including the subheader and portions have been rearranged. Additionally, the researchers have since adjusted key infographics to improve the source material's clarity, which has been added to this article.
In 2021, approximately 2 million unnecessary healthcare services were delivered, leading to $134 million in superfluous healthcare spending, according to an analysis from the Center for Improving Value in Health Care (CIVHC).
“This most recent analysis puts crucial information into the hands of the people who need it most,” Kristin Paulson, president and chief executive officer of CIVHC, said in the press release. “Understanding the most frequent low value services occurring in Colorado and how much they cost can help health insurance companies, providers, and patients work together to improve care and lower costs.”
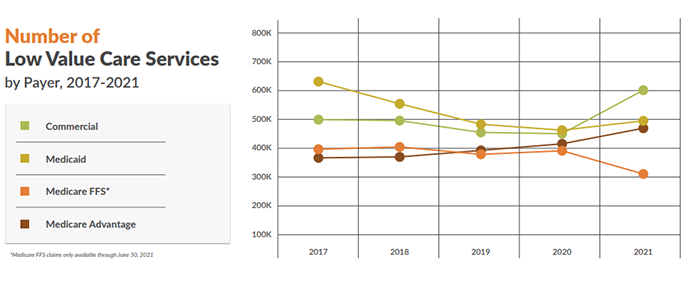
The analysis leveraged 2017 to 2021 claims data from the Colorado All Payer Claims Database (CO APCD). Researchers analyzed the data using Milliman’s MedInsight Health Waste Calculator, assessing the frequency and cost of 58 potentially low-value care services.
The top five low-value services were opioid prescription, Vitamin D deficiency screening, prostate cancer screening, imaging tests for eye disease, and coronary angiographies. Together, these services contributed almost two-thirds of Colorado’s overall low-value care spending (63 percent).
Opioid prescriptions for chronic pain unrelated to cancer cost $47.9 million, the highest unnecessary spending. Vitamin D deficiency screenings cost $12.4 million, and the remaining three services each contributed less than $7 million to unnecessary healthcare spending.
The average cost of a low-value service was $70 per instance. Some services were severely expensive, such as one proton beam therapy service, which can cost $19,000.
The unnecessary spending tracked in this analysis did not include the downstream excessive spending resulting from irrelevant and even harmful procedures. For example, unnecessary opioid prescriptions cost the system $47.9 million, but this does not include the later costs for opioid addiction treatment or overdose-related deaths.
Five types of Colorado insurers contributed to the database: Medicaid, Child Health Plan Plus (CHP+), commercial plans, fee-for-service Medicare, and Medicare Advantage.
Overall, the share of healthcare spending that qualified as one of the 58 low-value services declined over time. In 2017, the share fell between 8 and 9 percent, but by the end of June 2021, it fell to around 7 percent.
The payers that were most likely to spend on low-value services were commercial health plans. In these plans, the highest unnecessary spending occurred for inappropriate opioid prescriptions ($12.5 million), routine general health checks ($3.4 million), and vitamin D deficiency screenings ($6.8 million).
Fee-for-service Medicare spent on colorectal screenings in adults 50 years and older ($8.6 million), prostate cancer screenings ($2.3 million), and prescribing two or more antipsychotic medications ($1.8 million). Medicare Advantage spent a staggering $13.6 million on inappropriate opioid prescriptions as well as $2.5 million on vertebroplasty and $1.7 million on colorectal screenings in adults 50 years and older.
“Interestingly, Medicare Fee-for-Service and Medicare Advantage, payers that typically cover the same age groups, do not have the same top three low value services by spend with the exception of colorectal screenings in adults over 50,” the press release noted. “This may be due to differences in coverage and/or reimbursement rates.”
CHP+ unnecessarily covered screenings for Vitamin D deficiency ($177,000), CT scans for abdominal pain in children ($163,000), and pediatric head computed tomography scans ($108,000). In Medicaid, the most expensive unnecessary services were inappropriate opioid prescriptions ($12.9 million), Vitamin D deficiency screenings ($4.2 million), and prescribing two or more antipsychotic medications ($1.4 million). Separate research has found that Medicare Advantage plans spend less on low-value care services than fee-for-service Medicare due to its embracing value-based care.
An accompanying issue brief recommended that payers evaluate their payment models and incentivize providers to move away from low-value care services.
Experts have recommended leveraging existing lists of low-value care services—such as those provided by CIVHC, Choosing Wisely, and USPSTF— to identify low-value services. Levers that can reduce low-value care include alternative payment models, aligning out-of-pocket costs, and joint ventures between payers, providers, and social agencies.