
Getty Images/iStockphoto
Time, Commitment Required for ACO, Value-Based Care Success
Accountable care partnerships will need to have greater patience when it comes to earning shared savings.
In healthcare, as in so many other areas of life, patience is a virtue. Providers and payers pursuing ACO development will need to have plenty of it before their care transformation efforts pay off with significant cost savings.
As providers combine growing financial incentive opportunities with improved population health management programs, they may be able to achieve many of the goals of healthcare reform.
But accountable care organizations will need to show commitment and perseverance if they are to reap the benefits of value-based care.
Experience breeds results for accountable care organizations
“True transformation is a long-term endeavor,” said Amy Oldenburg, Vice President of Network and Product Strategy Accountable Care Solutions at Aetna. “We know that it takes at least three years for motivated ACOs to make changes necessary to impact real savings and quality improvements.”
CMS, which is leading the most aggressive push toward accountable care, acknowledges that the longer an ACO is in operation, the greater the savings they generate.
Recent data confirms this assessment. Pioneer Accountable Care Organizations were able to garner more cost savings during their third year of operation than their first year.
Data from the Brookings Institution points out that the Pioneer ACOs accrued $96 million in savings in their second year of operation, compared to just $87 million in their first twelve months.
“We know that it takes at least three years for motivated ACOs to make changes necessary to impact real savings and quality improvements.”
“We are seeing the same savings trend, and like CMS, we intend to stay the course,” Oldenburg emphasized.
“We believe transforming health care will help reduce waste, improve quality, improve member/patient satisfaction, and improve overall employee health and productivity,” Oldenburg added. “So we see this as well worth the commitment and investment of time and resources to get there. Through our approach to move providers and hospitals toward full, product-based risk-sharing ACOs and helping them transform the way they do business, we know we can help build a healthier world.”
One way to ensure providers can generate cost savings over time is for accountable care organizations to pursue risk-based payment arrangements aimed at rewarding quality performance benchmarks.
Read: The Future is Accountable Care, Population Health Management
Once accountable care organizations move into risk-sharing and risk-assumption arrangements, the potential for cost savings increases, according to Mark Wagar, President of the Heritage Provider Network.
“While they need to be careful about assuming more risk, I think the biggest thing for ACOs is to be more aggressive,” Wagar said. “There are too many healthcare organizations with potential that are sitting on the sidelines and saying ‘Let’s do just shared savings because we can’t lose. We will bill for fee-for-service and if we happen to improve things, we get a bonus but otherwise, we don’t lose.’”
“While that may be a comfortable spot for healthcare organizations that aren’t familiar with value-based care in its more mature forms, it limits how much they can really control decision-making.”
“Particularly if you’re a physician-driven organization like Heritage, it’s very important to assess best practices quickly, put them into effect quickly, and be candid with your physicians and the entire delivery system about best practices, disparities between different delivery systems, and ways to get the best outcome.”
“I think there is potential positive news with the movement of the federal ACOs toward risk-sharing and risk-assumption,” Wagar asserted. “When we got into our Pioneer ACO, we were one of the first and we’re still staying in it and will move onto the next phase because we want to help demonstrate that independent practices as well as our large group organizations can have impact.”
When health payers and accountable care organizations partner to form risk-based contracts with a focus on value-based care payments, the quality of healthcare services is expected to increase.
However, the Medicare Shared Savings Program may not be meeting the expectations of many within the healthcare industry. The way this program succeeds is by having more ACOs take on shared risk, but some accountable care organizations have been dropping out of MSSP because they weren’t achieving the monetary savings they once hoped to reach.
“I think there is a way to meet the goals of the program, but they’re going to have to keep evolving the payment policy to a more truly value-based and population-based payment rather than try to keep making something out of fee-for-service,” Wagar said.
“You have a lot of elements that still would rather not move in that direction [toward value-based care payments] because they’re afraid of moving off on their current approach to their business side. But it has to happen. We can’t keep using the same payment method that would otherwise be unnecessary if we’re able to apply a best practice.”
Engaging in the value-based reimbursement revolution can produce positive results. For example, the latest data from the MSSP and Pioneer ACO programs shows savings of $817 million for the healthcare system.
Pioneer ACOs produced a 1 percent greater reduction in healthcare spending when compared to fee-for-service programs within their first two years. MSSP ACOs were able to reduce healthcare costs by about 1 percent, as well, and generate shared savings of more than $300 million by 2014.
Accountable care organizations may bring cost savings to commercial insurers as well as Medicare and Medicaid, says Ted Schwab, Managing Director at Huron Healthcare.
“There’s no question about it,” he stated. “I think that there has been some question to date because of the failure of Pioneer ACOs and the regular MSSP ACOs to show much cost savings but what folks have overlooked is that the ACO movement has been an organizing force throughout the healthcare industry and it’s got hospitals and doctors for once under the same umbrella talking about efficiencies, clinical protocols, and ways to save costs.”
"We can’t keep using the same payment method that would otherwise be unnecessary if we’re able to apply a best practice.”
“There are now north of 700 of these organizations in the United States of America. If you think about where the industry has been for the last 100 years, it’s been a mom-and-pop fragmented industry. Now you have 700 organizations with folks at least talking to each other. It’s going to take a while.”
“We’re at the very beginning of this movement and I could not be any more encouraged,” Schwab added.
Gregory Scrine, Managing Principal at healthcare consulting company Lumeris, also believes finds that value-based payment models can bring better patient care.
“Without a doubt, the industry is moving towards more value-based payment arrangements. Fee-for-service will never go away, but a growing portion of provider revenue streams and payer contracts will be value-based arrangements in some form or fashion,” Scrine said.
“So, does it improve quality? I believe that by definition, it has to. In the 1990s, we learned some valuable lessons about shifting risk. Providers lacked the ability to measure quality and the impact on quality and outcomes. Since then, we have made huge strides in understanding how to use data to define quality measures.”
“The Triple Aim Plus One target, which is better care at lower cost, better patient experience, and greater provider satisfaction is the path to value-based care. If done right, it creates a virtuous cycle where the right behavior and higher quality are rewarded, and it creates greater participation and incentive to move towards value-based care delivery.”
As value-based payment arrangements become a staple in the payer industry, fee-for-service payment models are likely to grow less popular. The trend is already evident, says Oldenburg.
“The industry has embraced value based contracting with CMS leading the path,” she said. “The majority of carriers have publicly stated current VBC penetration, defined as percentage of spend in value-based contracts, as well as targets by specified time periods. Aetna has targeted 75% of our spending to be in a value based contract by 2020.”
“Value-based contracts align incentives amongst the provider community. Providers are rewarded for the overall management of the population. The focus is on ensuring the quality of care which over time leads to lower costs through reduction in things such as waste and inefficiency.”
How federal incentives play into cost reduction
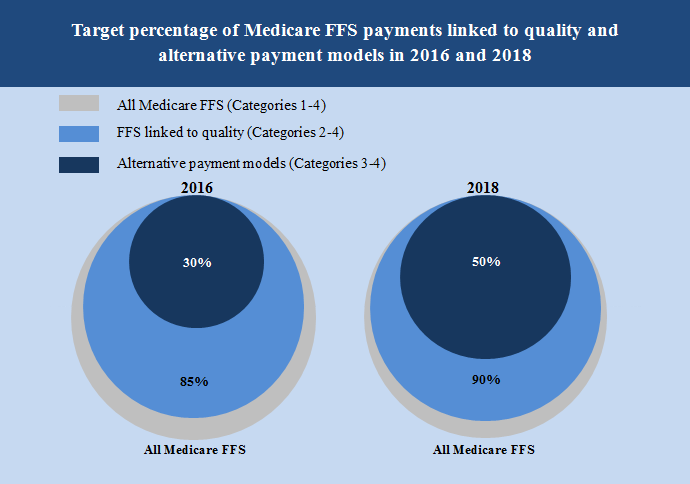
CMS has set out a goal of moving 30 percent of Medicare reimbursement into alternative payment models including bundled payments by the end of 2016 and 50 percent of Medicare reimbursement toward alternative payment by the end of 2018.
“Payment models, not unlike contracting models, can be thought of as a continuum of options,” Oldenburg explained. “Providers are at varying levels of readiness to accept payment models that include additional risk including bundled payments and global capitation. That being said, we do see providers who are looking to contract under more advanced payment models.”
“Valued based contracts will continue to increase in penetration. Providers who have entered into more basic forms of value based are likely to move up the continuum and accept additional risk over time,” she continued. “We will continue to partner with providers on the transformation of their practices which will include delegation of traditional carrier activities directly to the health system.”
Population health management assists ACOs in cutting costs
A strong focus on population health management is required for ACO participants to produce shared savings. However, execution of these strategies remains a problem that may ACOs still need to solve, says Scrine.
“While it is fairly well-understood what needs to get done, execution remains the hard part. It goes back to having those five elements in place: organizational design and leadership governance; organizational structure; the Triple Aim Plus One; a payer strategy and an informatics infrastructure.”
Read: Physician Leadership Key to Accountable Care Organizations
Smaller accountable care organizations may be able to achieve stronger and more effective population health management strategies through partnerships with more experienced organizations, he suggested.
“Partnerships with experienced organizations in the space can help organizations drive effectiveness of their execution and their strategies,” he stated.
“One of the ways to make those strategies more effective is to pursue scale. There’s lots of organizations that are approaching population health initiatives in somewhat of a small measure. The reality is, to be successful in the space, it requires an organization to take a relatively big swing to move the needle and make progress in these efforts. With that bigger swing comes more risk.”
When asked about how Heritage Provider Network developed their population health management programs, Mark Wagar responded, “For one, maintaining and developing a robust database is necessary. The advantage we’ve had is it’s a physician organization creating the database and having the most impact.”
“[We store] any and all pieces of information about patients – their living circumstances, their social and economic circumstances. When all that comes together, we’re able to list profiles earlier than some organizations as a result and get information that’s actionable in the hands of our primary care physicians.”
“Partnerships with experienced organizations in the space can help organizations drive effectiveness of their execution and their strategies.”
“Our specialists collaborate with hospitals on a fact-based basis and about what would be most helpful to complex patients and their families who need lots of services. [A large database of patient information] could delay the onset of further complications, reduce severity, or eliminate them altogether in the future,” continued Wagar.
Storing key data about patient health and living situations could allow providers to prevent health issues from escalating and would, thereby, lower costs.
“It’s physician-owned and driven at Heritage, but we use all kinds of providers, care workers, and collaborate with local organizations. You have to pull all this together to really help a person in their total circumstance,” Wagar said.
“It’s not just that they have a bad hip. They may be elderly and may have five or six other complicating problems related to addressing the hip. There could be family situations.”
Population health management programs would benefit from the integration of social and behavioral health data. In 2014, the Institute of Medicine suggested that healthcare providers include behavioral health statistics in electronic patient records as a way to develop a more holistic understand of the patient and his or her situation.
Last year, in a policy brief, the American Academy of Nursing also encouraged the inclusion of social and behavioral health data in electronic patient records so that health IT systems contain the information necessary for a robust population health management program.
“I think we made a mistake years ago as a healthcare industry in carving out behavioral health because it’s so integral to medical health,” said Wagar. “You find out different things that you don’t find out in the traditional delivery system.”
“You might have wonderful offices and facilities and you’re waiting to take good care of somebody when they fall and injure themselves, but you haven’t discovered the thing that could have prevented that altogether or lessened its severity. That’s the biggest difference – we’re enabling our physicians and other providers to be proactive rather than just wait for people to show up when they feel they are in bad shape and need to see somebody.”
Patient engagement is also key for producing better outcomes and cutting costs. Platforms aimed at changing lifestyle choices and improving healthy decision-making may reduce the likelihood of some chronic disease and ultimately lead to lower healthcare spending.
Last year, CMS began a five-star ratings program in which patients can choose the hospitals with the highest patient satisfaction rates through Medicare’s Hospital Compare website. But federal records show that hundreds of hospitals have still not achieved real improvement in their patient satisfaction ratings, despite implementing more patient engagement technologies.
“There’s lots of information and data that patient satisfaction throughout the healthcare industry is not very good,” Schwab admitted. “We’re starting at a pretty low base. There is some interesting information coming out of clients that those who are organized around ACOs, patient satisfaction goes up, patient engagement goes up, and by far, they have much better clinical outcomes.”
“All of that will build eventually to tremendous cost savings but we’re just at the beginning of that.”
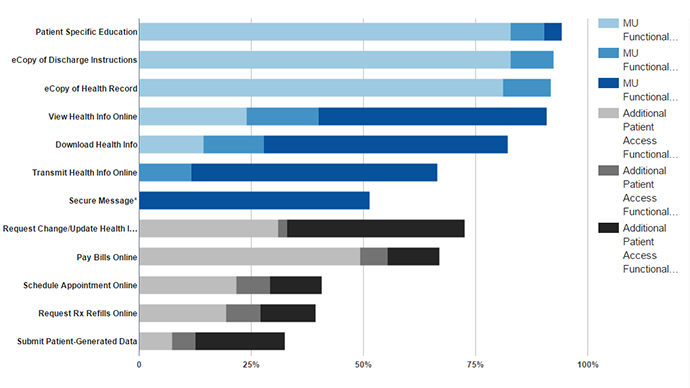
Patient engagement may increase when payers implement portals for their members. Greater interoperability between provider and payer patient portals could also lead to a rise in patient satisfaction and engagement, explained Brooke Nordai, Director of Product Innovation at Capital Blue Cross.
“Customers can access a personalized portal and a variety of tools through our website,” she said. “Capital BlueCross is not yet seeing interest from customers to launch patient portals. Most of our customers access their personal health information through their physician’s patient portal as opposed to their health plan. For this to become real on the insurer side, more integration needs to occur with health systems and providers.”
“We offer tools on our member portal to engage customers in making more informed healthcare decisions, including searching for providers and looking for quality and cost information for services and medical procedures,” Nordai continued.
“If I’m having an elective service done like an MRI or CT scan, I’m able to go out and use those consumer principles and shop for a physician. I might be in a high deductible plan, so with a large deductible, I want to make sure I’m using my money to the best of my ability just like I would do in other consumer decisions.”
Cost transparency is becoming a more popular topic throughout the healthcare industry as consumers and federal agencies continually look for ways to cut spending. Payers who include member portals with provider pricing information may be able to deliver the cost transparency many consumers seek.
“Our goal is to simplify the complex healthcare system through consumer tools that aid in the decision making process for our customers,” Nordai said.
When asked about the future of the health insurance industry and what trends payers should pay attention to, Nordai answered, “Consumerism is at the center of the rapidly evolving healthcare industry. Historically, our business was primarily business-to-business. Now, with the influx of individuals buying their own health care coverage, either on or off the federally-facilitated marketplace, we need to change our mindset and service model to be more relevant to the individual consumer.”
“How we interact with and engage individual customers requires a different approach than our relationships with our commercial customers, though there are similarities in expectations from both. Industries like banking and real estate have paved the way for us in how they evolved to make it easy for their individual customers to access the information they want through websites and portals. I think we are well on our way on this journey, and healthcare will become much more transparent in the next couple of years.”
Achieving success in accountable care
Accountable care partnerships will need to have greater patience when it comes to earning shared savings in either payer-provider contracts or through CMS programs. It often takes three or more years before most ACOs are able to decrease costs by a significant level.
Over several years of operation, many ACOs show greater quality improvement and lower healthcare spending, which illustrates how important experience and commitment are to the success of accountable care organizations. As accountable care organizations and value-based arrangements mature, the medical industry should be able to see a drop in healthcare spending.






