
Getty Images/iStockphoto
Key Strategies for Transitioning a Health Plan into Cloud Computing
Cloud computing technology adoption is on the rise worldwide, but how can health plans shift their complex processes into this new platform?
Updated 08/14/2023: This article has been updated to reflect a few timeline discrepancies. Additionally, Lisa Davis's position was formerly listed as "senior vice president," which was her role when she was hired at Blue Shield. Her title has been edited to specify her current position: executive vice president.
When Lisa Davis started her position as senior (now executive) vice president and chief information officer at Blue Shield of California (Blue Shield) in February 2020, the company was still blending its cloud computing solutions with an on-premises system. Hybrid cloud computing and on-premises systems were common in the payer space, but relied on outdated technology.
At Blue Shield, the on-premises system had 1,200 connected batch jobs. These automated tasks focused on moving data from one system to another in a compliant manner, enabling timely responses to members and providers. But it took months to complete the billions of transactions that the payer needed to process.
Then, the pandemic struck. Davis, with Blue Shield, joined California’s Vaccine Task Force in May 2020. She saw public health officials scramble to distribute coronavirus vaccines in an equitable, timely way using antiquated systems.
For Davis and the public and private payer entities she served, the coronavirus pandemic highlighted all of the inefficiencies of their systems. It was the wake-up call that summoned healthcare organizations away from outdated technologies and into cloud computing.

Worldwide, businesses flocked to cloud computing solutions during the pandemic and in its aftermath. Public cloud services spending globally was expected to jump 21.7 percent from 2022 to 2023, according to Gartner. By 2026, three-quarters of all businesses worldwide are expected to have a cloud-based platform.
Although Blue Shield had partially integrated cloud technologies, Davis ushered Blue Shield into the movement and kickstarted the company's cloud-first strategy. Blue Shield partnered with Microsoft to launch two projects that would initiate this transition.
First, the partners created Blue Shield’s Experience Cube which compiles payer, provider, and member data to create more efficient, near real-time data exchange using the Microsoft Azure cloud platform. The initial use case will be a digital health record that includes a large spectrum of information from lab results to social determinants of health data.
Additionally, Microsoft and Blue Shield are working toward cloud-based transactions. Using Microsoft Azure, the health plan transitioned an automated software solution into the cloud.
As Blue Shield committed to this strategy, Davis identified a few key benefits and challenges associated with this transition that payers should be aware of as they consider cloud computing solutions.
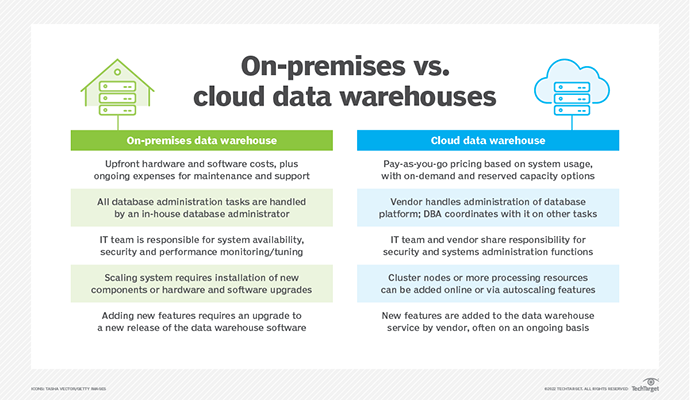
On-premises versus cloud computing
With on-premises (on-prem) infrastructure, the company has full control over the hardware and systems. The system requires the organization to have the correct hardware on site.
Cloud computing operates differently. There are three types of cloud service models.
Software as a Service (SaaS) users access the cloud via the internet and the service provider maintains the software. Platform as a Service (PaaS) allows developers to customize the applications while the service provider manages the rest (servers, storage, and network).
Lastly, Infrastructure as a Service (IaaS) cloud vendors host all of the on-premises infrastructure at a separate site and users access the services via the internet.
Why payers move from on-premises systems to the cloud
One of the major benefits of moving to cloud computing was the ability to scale the solution, both across members and providers. Scaling up an on-premises infrastructure is much more complicated, Davis explained.
Agility also drives payers toward cloud computing. In the cloud, payers pivot to meet market needs and member and provider demands more quickly. This could improve transforming certain processes to comply with regulatory changes, capturing an emerging share of the market before competitors, or transitioning to online platforms.
Real-time data exchange grows increasingly necessary in the healthcare space. On-premises systems cannot offer real-time data or even near real-time data in many cases.
Complying with regulations while also gathering data across the healthcare system to reply to members and providers in a timely manner with an infrastructure that had 1,200 batch jobs connected together could not result in instant data exchange, Blue Shield found.
“At the heart of our strategy of moving to the cloud is the data—data interoperability, data sharing, and getting that data in near real-time,” Davis said.
“We can improve the quality of care for our members, we can engage with our providers better, [and] we can make better decisions around the cost of healthcare because we have that information right at our fingertips. And you need the infrastructure to be able to support that.”
Innovation is at the core of payers’ decisions to move to the cloud. The solution allows payers to effortlessly update their systems, helping them remain current. Any changes and updates are interwoven into the system by the cloud technology partner.
For example, many cloud platforms now offer artificial intelligence and machine learning support that is seamlessly integrated into the system, allowing payers to remain up-to-date technologically without having to do a hardware overhaul.
Lastly, payers choose the cloud over on-premises solutions for the cloud’s cybersecurity capabilities.
Healthcare data breaches doubled between 2016 and 2021, according to the Department of Health and Human Services (HHS), and cloud systems are susceptible to these attacks. However, the strength of a cloud system’s cybersecurity increasingly depends on the users’ awareness and security ownership, as opposed to the security capabilities of the cloud service provider.
Davis advocated for the widespread adoption of cloud computing.
“At this point, every company should be a cloud company because every company is a technology and data company,” Davis explained.
Challenges of cloud computing adoption
However, like any solution, cloud computing has its challenges.
The healthcare system’s complexity is a major barrier that payers face as they try to break into cloud computing. On the consumer level, this barrier leads to low healthcare literacy and higher unnecessary care utilization.
On the payer side, healthcare’s complexity can inhibit innovation. Over half of payer technology leaders indicated that lack of a fixed vision and disparateness from mergers and acquisitions have contributed to challenges in digital transformation, according to Deloitte. Cloud computing is no exception to these barriers.
Additionally, Davis noted that acquiring or upskilling the talent needed to use cloud technologies can present challenges. Payers must create a talent strategy to move their workforce from mainframes to the cloud.
The initial costs of transitioning to the cloud are high, although long-term costs may be lower.
The upfront price tag can be prohibitive for many organizations, stalling their entry into cloud computing or preventing them from achieving their cloud-related goals. Nearly four in ten business executives in healthcare stated that budgeting and investment constraints bar them from seeing measurable results from their cloud technologies (38 percent), a PwC report found.
Healthcare business executives also found that effectively measuring and quantifying return on investments and lack of cyber and privacy controls presented problems in cloud adoption (38 percent and 33 percent, respectively), the report added.
Cloud-first strategies
After committing to a cloud approach in 2021 and initiating a hybrid model, Blue Shield has transitioned to a cloud-first approach which continues to unfold in the pandemic’s wake. The company’s IT leaders mapped out a five-year plan to move from on-premises systems to an entirely cloud-based environment by 2027. Throughout this process, a couple of key strategies came to light.
Align cloud and business strategies
For payers to move into the cloud computing space, they need to align their cloud strategy with their business strategy.
Primarily, ensuring alignment means integrating clinical stakeholders and listening to their primary goals. It entails viewing technology and data as enablers of the strategy and tools for the overarching mission. When payers understand their clinicians’ priorities, they can better position these tools to serve those aims.
Create the right team
Moving into cloud computing may require new hires and partners as well as reformed strategies for upskilling current employees.
Payer leaders need to ask themselves: who are the right partners for this work? The best partners will align with the payer’s strategic principles. They will understand the company’s mission, priorities, and timeline.
These are good qualities to have in any technology partner, but they are especially necessary for an effort as massive as transitioning from on-premises to cloud computing.
Again, partnering with clinical stakeholders will be essential to forming a strong cloud transition strategy and building the right team to execute it. Payers should make transitional decisions with their clinical partners, keeping their members and their clinicians at the center of their decision-making approach.
Prioritize well
To put all the pieces in place for a successful transition to the cloud, payers need to prioritize tasks effectively. To assess the top goals, health plan leaders can ask themselves what functions will deliver the biggest return on investment, improve member experience, or boost health outcomes.
Based on their answers to these questions, they can assess which data and platforms should be the first to transition to the cloud.
Blue Shield’s strategy charts out a transition that spans four years. Davis knew that the highest priority was clinical quality. This included provider quality of care, the quality of the payer’s data, and the quality of interactions with members and providers.
Additionally, Blue Shield’s goal was to create a personalized, holistic, high-tech, high-touch member experience, complete with social determinants of health data.
As a result, the first Blue Shield data to shift into the cloud was clinical quality data. The payer moved all of its claims data into its technology partner’s data platform. At the time of this publication, Davis and her team were discussing use cases with the technology partner, such as what data sets would enable the health plan to implement a cloud-based digital health record.
Prioritizing well can empower payers’ ongoing discussions with their technology partners as they organize transitions to the cloud.
With aligned strategies, the right team, and clear priorities, payers can lead the healthcare industry’s movement toward cloud computing.







