
Getty Images
How Payers Can Launch a Virtual-First Health Plan
Virtual-first health plans appear to be the natural next step in the evolution of virtual care, remote care, and telehealth technology. How can payers launch a successful plan?
E-triage, telemental and telebehavioral healthcare tools, e-prescribing, virtual urgent care—in one year, these digital healthcare tools and many more transformed from somewhat obscure, non-integrated technologies to nearly ubiquitous modes of healthcare delivery. Now, payers are using virtual-first health plans to continue innovation.
CMS approved 80 new types of telehealth services in 2020, according to a McKinsey & Company report, demonstrating both the boom in telehealth innovation and regulatory relaxation toward existing telehealth solutions.
With 2020 consigned to history, health insurers have to decide how to organize this constellation of emerging and evolving telehealth and virtual care tools into a robust backbone for healthcare management.
To do this, many payers are turning to virtual-first health plans.
“Telehealth and virtual are tools in the toolkit of innovating around healthcare,” Oleg Bestsennyy, partner at McKinsey, told HealthPayerIntelligence. “The pandemic has been obviously a huge tragedy to society, but the one thing that it did lead to is squeezing what would normally take decades of adoption of telehealth and virtual care into literally a space of a few months.”
“We definitely think virtual is here to stay long term,” Jennifer Rost, partner at McKinsey, confirmed to HealthPayerIntelligence.
The question “what does the future hold for virtual-first health plans?” generated a lot of excitement for Bestsennyy and Rost as well as Dawn Maroney, president of markets at Alignment Healthcare, and Marianna Spanos, general manager and vice president of virtual care at Oscar Health.
However, before payers can start to think about what virtual-first health plans could mean for the future, they have to define what these plans are in the present.
What is a virtual-first health plan?
Due to its newness, experts are still discussing the definition of a virtual-first health plan. However, some common factors are starting to emerge.
“Virtual first health plans are defined as health plans where the first entry point to getting medical care is with a virtual provider, typically primary care, often much more with a longitudinal relationship versus an on-demand provider,” Rost explained.
“The line in the sand of ‘what does virtual first plan mean’ is that the first interaction with a provider of record is conducted virtually,” Bestsennyy added.
Rost and Bestsennyy drew a distinction between a virtual-first health plan and a virtual care benefit.
“We're seeing both health plans and providers coming out with what I would define more as a virtual first benefit where the same type of access to virtual providers is available, but not a required feature of the health plan,” Rost clarified.
For example, the “digital front door”—or the digital starting point that transitions patients to their next point of care—is a virtual care benefit.
A virtual health plan will likely include an AI platform or telehealth visit as its digital front door to usher members into the various benefits that the plan may offer. However, the McKinsey researchers were careful to distinguish this as a component of a virtual health plan and not synonymous with the health plan itself.
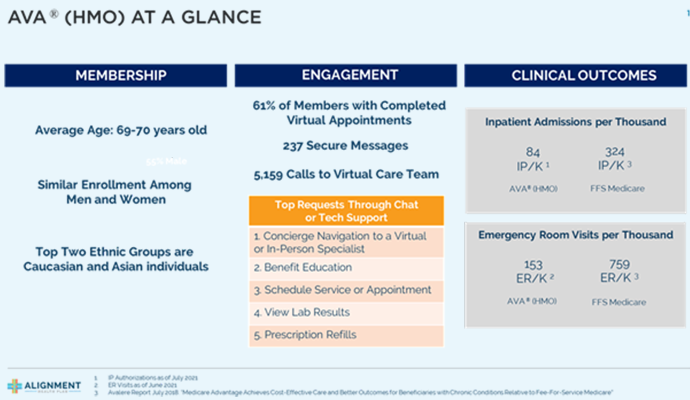
An example of this type of plan is Alignment Healthcare’s virtual-first Medicare Advantage plan, which is a health maintenance organization (HMO) product. The plan uses a concierge-style service that is available 24/7 through its ACCESS On-Demand Concierge platform.
The payer’s internally-developed technology platform, Alignment’s Virtual Application (AVA), supports its virtual-first health plan by pulling real-time patient data to construct a “patient 360” report, which offers a holistic view of the member’s condition.
Not all experts are aligned on whether a virtual-first health plan requires virtual care as the first step to receiving care and the definition is still crystalizing.
For example, Oscar Health’s definition of a virtual-first health plan is slightly broader.
“Our virtual health plans very prominently feature our virtual primary care offering, which includes $0 access to virtual primary care. And then they go further than that, in that they have additional benefits built into the plan design through incentives around labs and medications, where basically if your virtual provider prescribes and orders one of those services, we also waive cost-shares on those services,” Spanos shared with HealthPayerIntelligence.
“We do not necessarily require a member to use that virtual primary care service. It's not an HMO, so they're not required to go through a primary care provider, whether virtual or non-virtual, and they don't have to interact with virtual primary care. But the entire plan design does encourage the member to use that virtual primary care, and also includes other plan design elements that link to that primary care offering.”
Oscar Health’s virtual-first options span their virtual primary care benefit and virtual urgent care benefit.
The definition and benefits of a virtual-first health plan are still evolving as payers figure out how to design them, but many can agree that the plans carry certain advantages over traditional offerings.
Advantages of starting a virtual-first health plan
Bestsennyy outlined four primary benefits of a virtual-first health plan. Virtual-first health plans:
- Are more convenient
- Lead to higher quality of care
- Lead to better outcomes through better preventative care
- Reduce costs due to efficiency

The convenience of leveraging virtual care as the first point of care can manifest in time saved on transportation, decreased barriers to access related to stigmas, and more.
The format also gives members more control over their healthcare management.
“The opportunity just to start at least the full patient 360 view through a virtual platform is critical because it can be scheduled by that consumer directly,” Maroney said.
By giving members more control and making it more convenient, some leaders in the field are expecting to see better patient outcomes.
“We know that good preventative care, active management of chronic health conditions, that's really pretty critical to improving our members’ health outcomes,” Spanos said.
“But we also know that a lot of our members aren't accessing primary care regularly. There's a shortage of primary care providers in the US. There's also no guarantee that the time and place of those appointments will be convenient for our members.”
As a result, many patients resort to high-cost care sites, such as emergency departments.
By offering an alternative through integrated virtual care, experts are hoping to see better patient outcomes and reduced costs. However, since the virtual-first health plan is still so new, there is not a lot of hard data to disprove or support that hypothesis.
Rost noted that a previous McKinsey analysis discovered that switching from emergency department care to virtual urgent care could reduce the cost of a visit from thousands of dollars to only $50. But, Bestsennyy qualified, improved convenience can also create the potential for waste, and that potential outcome has yet to be quantifiably measured.
After only eight months post-launch, it was still too early for Oscar Health to be able to share any cost savings that the payer has seen with its virtual primary care benefit. However, Spanos pointed to other results that could indicate areas in which virtual care will produce savings for the payer.
For example, the health plan is seeing 80 percent first-fill medication adherence for medications that Oscar Health’s virtual care providers prescribe. Furthermore, Oscar Health’s virtual primary care providers have proven to be 24 percent less likely to prescribe high-cost drugs when a lower-cost drug option is available.
“So now you start to create the downstream cost outcomes that we want to see, in addition to actually driving the member behavior that we want to see around adherence,” Spanos shared.
“A lot of these results are driven by the plan designs, the member experience around virtual care, and then the deeply integrated data and information flows across our clinical platforms and our claims platforms.”
"A lot of these results are driven by the plan designs, the member experience around virtual care, and then the deeply integrated data and information flows across our clinical platforms and our claims platforms."
Overcoming top challenges
Despite many benefits, virtual-first health plans still encounter many challenges, especially since telehealth utilization is still stabilizing after the last year. One of the challenges that virtual-first health plans face is a lack of utilization.
Consumers are largely on board with integrating digital tools into healthcare. According to the McKinsey report, between 40 and 60 percent of consumers said that they were interested in a virtual-first health plan or components of the virtual-first health plan, like the digital front door.
However, health plans often find that consumers who express enthusiasm about digital options may not actually utilize those tools once they are available, the McKinsey report stated.
“For the initial adoption, you're truly looking for early adopters,” Bestsennyy explained. “US healthcare consumers are in this bucket where a majority of them are interested in products like this, but aren't true early adopters.”

Recognizing this trend, Rost and Bestsennyy emphasized a couple of steps that virtual-first health plans can take to help boost actual utilization of virtual care benefits.
First, insurers can continue to hone their member engagement and communication strategies to ensure that members know what virtual-first health plan benefits are available and how to use them, Rost recommended.
These efforts should go beyond email or paper mail alerts to inform members about the digital tools at their disposal. Insurers should aim for greater personalization and active, well-timed nudges.
Member engagement and communication were areas that pulled down payer consumer satisfaction ratings in 2020, so this should already be an area that they are attempting to improve.
Second, insurers should make sure the consumer’s experience is seamless in order to facilitate utilization.
Consumers should not have to click through multiple apps or links in order to get to the information or tools that they want. Retail and banking apps set an excellent standard for this strategy, Rost indicated.
Payers’ existing interoperability compliance efforts can be key to seamlessly integrating digital tools in a virtual-first health plan, according to Bestsennyy. For an effective virtual-first health plan, data should flow easily and securely between the virtual care provider and in-person provider, especially if they are two separate individuals or entities.
“We've invested a lot into integrations to make sure that it's easy to get your lab work done, that it's easy to get your medication delivered to the home. And so that's an area where I'm really excited to continue innovating because I don't think it's an easy problem to solve, but it's one that we've invested in pretty heavily right now,” said Spanos.
Third, Bestsennyy pointed out that coordinating with providers is key to improving member uptake.
“A lot of consumers act based on recommendations of providers, so a lot of it depends on providers recommending and nudging them towards such solutions,” Bestsennyy said.
Health plans engage providers in virtual-first health plans in a variety of ways in order to enable a seamless experience for members.
“A lot of consumers act based on recommendations of providers, so a lot of it depends on providers recommending and nudging them towards such solutions.”
Some virtual-first health plans are coming from insurers with integrated delivery systems, Rost pointed out. In these systems, the provider that a patient meets with virtually is the same provider that she would meet with in-person. This model of engaging providers creates a sense of continuity between virtual and in-person care.
When the virtual care providers are not from within the payer’s provider network but rather are attached to a telehealth provider, payers have to engage with the telehealth provider to ensure that they are pursuing longitudinal care.
Instead of the telehealth provider offering one-time care, they work toward building a relationship with each patient. This is particularly important for virtual-first health plan members who do not have an in-person primary care provider. If successful, this strategy can be key to developing a seamless model.
However, outside of these two approaches, payers are still exploring how to meaningfully engage their existing provider partners outside of integrated delivery systems in payers’ virtual-first health plans. According to Rost, this is still a space that is evolving and requires more attention.
Fourth, in order to increase utilization among members, insurers can offer incentives.
Many new virtual-first health plans highlight zero-dollar copays on certain digital services and highlight the lower costs of these virtual-first health plans overall. These financial perks are effective, not only for drawing in users, but also for boosting utilization.
Supporting early adopters with technology challenges
The virtual-first health plan is not for everyone—at least, not yet. Securing a strong consumer base will be key to the model’s survival and growth.

One key barrier to becoming a virtual-first health plan early adopter is access to technology. Maroney has seen this within the Medicare Advantage community that Alignment Healthcare’s virtual-first health plan serves.
“Not everybody is ready for this. You have people that do not have technology but they love the richness of the product itself,” Maroney shared.
The cost savings associated with this model could help overcome some technology and WiFi access barriers. For example, at Alignment Healthcare, members receive $100 in over-the-counter drug benefits which they can use at their own discretion, including to pay for WiFi coverage, broadband access, or an iPad or AppleWatch purchase.
Apart from having technology access, individuals who are best suited to becoming virtual-first health plan early adopters desire greater control over their healthcare management.
Certainly, the health plan has a duty to actively engage its virtual-first health plan members, Maroney acknowledged. But the members who will get the most benefit out of this type of plan are the ones who are likely to initiate contact and engage regularly with their healthcare providers.
The first step for an Alignment Healthcare virtual-first Medicare Advantage plan consumer is to schedule their initial appointment. If the consumer does not proactively schedule it, Alignment Healthcare will nudge them to do so. This is the hardest step, Maroney said.
For virtual-first Medicare Advantage plan members who have the right technology but feel less comfortable using it to manage their healthcare, the team at Alignment Healthcare provides support and member education.
It starts with scheduling appointments for the member until he feels more comfortable. From there, the team continues to be proactive with the member to ensure that they feel supported.
The future of virtual-first health plans
Once payers have established the definition of a virtual-first health plan and confront the challenges of launching these plans, they can turn to the question that stirs up so much enthusiasm: What is the future of virtual-first health plans?

When peering into the future of the virtual-first health plan model, the horizon is still obscured by many unknowns.
“We're going to continue to see innovation in these health plans,” Rost said. “The trend is here to stay, and we'll see how much it stays close to the current path or continues to evolve from there.”
Bestsennyy expressed the hope that the future of virtual-health plans involves fusing the siloed worlds of virtual care and in-person care.
He pointed to the impressive amount of investments from principal investors--private equity from venture capital, funding from traditional payer and non-traditional tech giants, to name a few--as evidence of the value and innovation in this space. But this enthusiasm came with a word of caution.
“One of the warnings to the incumbents of the system, both on the payer and the provider side, is that this innovation may come from the new entrants, and the incumbents may wake up one day and say, ‘we're too late to the game,’” Bestsennyy said.
Despite this sense of urgency, healthcare’s pace likely will be no different than the trajectories of the retail and financial industries, Bestsennyy predicted. Even with the coronavirus pandemic’s impact, it could take a few years for these solutions to take hold.
“I am hopeful that five years from now we'll have a completely different discussion where this is becoming the norm,” Bestsennyy said.





